Related Research Articles

Kwashiorkor is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates. It is thought to be caused by sufficient calorie intake, but with insufficient protein consumption, which distinguishes it from marasmus. Recent studies have found that a lack of antioxidant micronutrients such as β-carotene, lycopene, other carotenoids, and vitamin C as well as the presence of aflatoxins may play a role in the development of the disease. However, the exact cause of kwashiorkor is still unknown. Inadequate food supply is correlated with occurrences of kwashiorkor; occurrences in high income countries are rare. It occurs amongst weaning children to ages of about five years old.

Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area may feel heavy, and joint stiffness. Other symptoms depend on the underlying cause.

Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein, less than 150 mg/day; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become foamy. Severe proteinuria can cause nephrotic syndrome in which there is worsening swelling of the body.

Ascites is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdominal size, increased weight, abdominal discomfort, and shortness of breath. Complications can include spontaneous bacterial peritonitis.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.

Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy urine. Complications may include blood clots, infections, and high blood pressure.

Serum protein electrophoresis is a laboratory test that examines specific proteins in the blood called globulins. The most common indications for a serum protein electrophoresis test are to diagnose or monitor multiple myeloma, a monoclonal gammopathy of uncertain significance (MGUS), or further investigate a discrepancy between a low albumin and a relatively high total protein. Unexplained bone pain, anemia, proteinuria, chronic kidney disease, and hypercalcemia are also signs of multiple myeloma, and indications for SPE. Blood must first be collected, usually into an airtight vial or syringe. Electrophoresis is a laboratory technique in which the blood serum is applied to either an acetate membrane soaked in a liquid buffer, or to a buffered agarose gel matrix, or into liquid in a capillary tube, and exposed to an electric current to separate the serum protein components into five major fractions by size and electrical charge: serum albumin, alpha-1 globulins, alpha-2 globulins, beta 1 and 2 globulins, and gamma globulins.
The globulins are a family of globular proteins that have higher molecular weights than albumins and are insoluble in pure water but dissolve in dilute salt solutions. Some globulins are produced in the liver, while others are made by the immune system. Globulins, albumins, and fibrinogen are the major blood proteins. The normal concentration of globulins in human blood is about 2.6-3.5 g/dL.

Anasarca is a severe and generalized form of edema, with subcutaneous tissue swelling throughout the body. Unlike typical edema, which almost everyone will experience at some time and can be relatively benign, anasarca is a pathological process reflecting a severe disease state and can involve the cavities of the body in addition to the tissues.
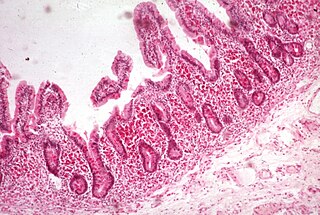
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety of anaemias.
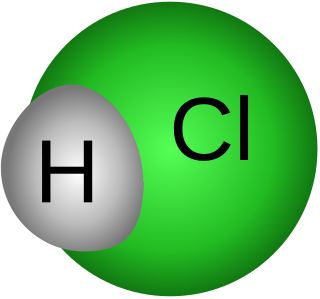
Achlorhydria and hypochlorhydria refer to states where the production of hydrochloric acid in gastric secretions of the stomach and other digestive organs is absent or low, respectively. It is associated with various other medical problems.
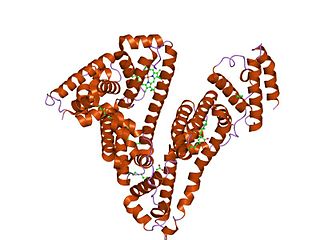
Serum albumin, often referred to simply as blood albumin, is an albumin found in vertebrate blood. Human serum albumin is encoded by the ALB gene. Other mammalian forms, such as bovine serum albumin, are chemically similar.

Minimal change disease is a disease affecting the kidneys which causes nephrotic syndrome. Nephrotic syndrome leads to the loss of significant amounts of protein in the urine, which causes the widespread edema and impaired kidney function commonly experienced by those affected by the disease. It is most common in children and has a peak incidence at 2 to 6 years of age. MCD is responsible for 10–25% of nephrotic syndrome cases in adults. It is also the most common cause of nephrotic syndrome of unclear cause (idiopathic) in children.

Hypoalbuminemia is a medical sign in which the level of albumin in the blood is low. This can be due to decreased production in the liver, increased loss in the gastrointestinal tract or kidneys, increased use in the body, or abnormal distribution between body compartments. Patients often present with hypoalbuminemia as a result of another disease process such as malnutrition as a result of severe anorexia nervosa, sepsis, cirrhosis in the liver, nephrotic syndrome in the kidneys, or protein-losing enteropathy in the gastrointestinal tract. One of the roles of albumin is being the major driver of oncotic pressure in the bloodstream and the body. Thus, hypoalbuminemia leads to abnormal distributions of fluids within the body and its compartments. As a result, associated symptoms include edema in the lower legs, ascites in the abdomen, and effusions around internal organs. Laboratory tests aimed at assessing liver function diagnose hypoalbuminemia. Once identified, it is a poor prognostic indicator for patients with a variety of different diseases. Yet, it is only treated in very specific indications in patients with cirrhosis and nephrotic syndrome. Treatment instead focuses on the underlying cause of the hypoalbuminemia. Albumin is an acute negative phase respondent and not a reliable indicator of nutrition status.

Lymphangiectasia, also known as "lymphangiectasis", is a pathologic dilation of lymph vessels. When it occurs in the intestines it is known as intestinal lymphangiectasia, colloquially recognized as Waldmann's disease in cases where there is no secondary cause. The primary defect lies in the inability of the lymphatic system to adequately drain lymph, resulting in its subsequent accumulation and leakage into the intestinal lumen. This condition, first described by Waldmann in 1961, is typically diagnosed in infancy or early childhood. However, it can also manifest in adults, exhibiting a broad spectrum of clinical symptoms.

Protein losing enteropathy (PLE) is a syndrome in which blood proteins are lost excessively via the gastrointestinal (GI) tract. It may be caused by many different underlying diseases that damage the lining of the GI tract (mucosa) or cause blockage of its lymphatic drainage.
Congenital nephrotic syndrome is a rare kidney disease which manifests in infants during the first 3 months of life, and is characterized by high levels of protein in the urine (proteinuria), low levels of protein in the blood, and swelling. This disease is primarily caused by genetic mutations which result in damage to components of the glomerular filtration barrier and allow for leakage of plasma proteins into the urinary space.
Glomerulonephrosis is a non-inflammatory disease of the kidney (nephrosis) presenting primarily in the glomerulus as nephrotic syndrome. The nephron is the functional unit of the kidney and it contains the glomerulus, which acts as a filter for blood to retain proteins and blood lipids. Damage to these filtration units results in important blood contents being released as waste in urine. This disease can be characterized by symptoms such as fatigue, swelling, and foamy urine, and can lead to chronic kidney disease and ultimately end-stage renal disease, as well as cardiovascular diseases. Glomerulonephrosis can present as either primary glomerulonephrosis or secondary glomerulonephrosis.
Waldmann disease, also known as Primary Intestinal Lymphangiectasia (PIL), is a rare disease characterized by enlargement of the lymph vessels supplying the lamina propria of the small intestine. Although its prevalence is unknown, it being classified as a "rare disease" means that less than 200,000 of the population of the United States are affected by this condition and its subtypes and there have been approximately 50 reported cases of adult-onset PIL since 1961.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/ml. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.
References
- ↑ Semrad, Carol E. (2012). "Approach to the Patient with Diarrhea and Malabsorption". Goldman's Cecil Medicine. pp. 895–913. doi:10.1016/b978-1-4377-1604-7.00142-1. ISBN 9781437716047. S2CID 78742479.
- ↑ "Hypoproteinemia: Symptoms, causes, and treatment". www.medicalnewstoday.com. 2019-12-10. Retrieved 2023-08-20.
- ↑ Laster, Leonard (1964-02-22). "Protein-losing Gastroenteropathy". JAMA. 187 (8): 227. doi:10.1001/jama.1964.03060210072030. ISSN 0098-7484. PMC 2482745 .