Ferritin is a universal intracellular protein that stores iron and releases it in a controlled fashion. The protein is produced by almost all living organisms, including archaea, bacteria, algae, higher plants, and animals. It is the primary intracellular iron-storage protein in both prokaryotes and eukaryotes, keeping iron in a soluble and non-toxic form. In humans, it acts as a buffer against iron deficiency and iron overload.

Lactoferrin (LF), also known as lactotransferrin (LTF), is a multifunctional protein of the transferrin family. Lactoferrin is a globular glycoprotein with a molecular mass of about 80 kDa that is widely represented in various secretory fluids, such as milk, saliva, tears, and nasal secretions. Lactoferrin is also present in secondary granules of PMNs and is secreted by some acinar cells. Lactoferrin can be purified from milk or produced recombinantly. Human colostrum has the highest concentration, followed by human milk, then cow milk (150 mg/L).

Total iron-binding capacity (TIBC) or sometimes transferrin iron-binding capacity is a medical laboratory test that measures the blood's capacity to bind iron with transferrin. Transferrin can bind two atoms of ferric iron (Fe3+) with high affinity. It means that transferrin has the capacity to transport approximately from 1.40 to 1.49 mg of iron per gram of transferrin present in the blood.
Transferrin saturation (TS), measured as a percentage, is a medical laboratory value. It is the value of serum iron divided by the total iron-binding capacity of the available transferrin, the main protein that binds iron in the blood, this value tells a clinician how much serum iron is bound. For instance, a value of 15% means that 15% of iron-binding sites of transferrin are being occupied by iron. The three results are usually reported together. A low transferrin saturation is a common indicator of iron deficiency anemia whereas a high transferrin saturation may indicate iron overload or hemochromatosis. Transferrin saturation is also called transferrin saturation index (TSI) or transferrin saturation percentage (TS%)

Human iron metabolism is the set of chemical reactions that maintain human homeostasis of iron at the systemic and cellular level. Iron is both necessary to the body and potentially toxic. Controlling iron levels in the body is a critically important part of many aspects of human health and disease. Hematologists have been especially interested in systemic iron metabolism, because iron is essential for red blood cells, where most of the human body's iron is contained. Understanding iron metabolism is also important for understanding diseases of iron overload, such as hereditary hemochromatosis, and iron deficiency, such as iron-deficiency anemia.

Hepcidin is a protein that in humans is encoded by the HAMP gene. Hepcidin is a key regulator of the entry of iron into the circulation in mammals.

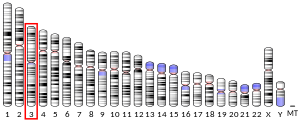
Human homeostatic iron regulator protein, also known as the HFE protein, is a transmembrane protein that in humans is encoded by the HFE gene. The HFE gene is located on short arm of chromosome 6 at location 6p22.2
Iron-binding proteins are carrier proteins and metalloproteins that are important in iron metabolism and the immune response. Iron is required for life.

Atransferrinemia is an autosomal recessive metabolic disorder in which there is an absence of transferrin, a plasma protein that transports iron through the blood. Atransferrinemia is characterized by anemia and hemosiderosis in the heart and liver. The iron damage to the heart can lead to heart failure. The anemia is typically microcytic and hypochromic. Atransferrinemia was first described in 1961 and is extremely rare, with only ten documented cases worldwide.

Transferrin receptor (TfR) is a carrier protein for transferrin. It is needed for the import of iron into cells and is regulated in response to intracellular iron concentration. It imports iron by internalizing the transferrin-iron complex through receptor-mediated endocytosis. The existence of a receptor for transferrin iron uptake has been recognized since the late 1950s. Earlier two transferrin receptors in humans, transferrin receptor 1 and transferrin receptor 2 had been characterized and until recently cellular iron uptake was believed to occur chiefly via these two well documented transferrin receptors. Both these receptors are transmembrane glycoproteins. TfR1 is a high affinity ubiquitously expressed receptor while expression of TfR2 is restricted to certain cell types and is unaffected by intracellular iron concentrations. TfR2 binds to transferrin with a 25-30 fold lower affinity than TfR1. Although TfR1 mediated iron uptake is the major pathway for iron acquisition by most cells and especially developing erythrocytes, several studies have indicated that the uptake mechanism varies depending upon the cell type. It is also reported that Tf uptake exists independent of these TfRs although the mechanisms are not well characterized. The multifunctional glycolytic enzyme glyceraldehyde 3-phosphate dehydrogenase has been shown to utilize post translational modifications to exhibit higher order moonlighting behavior wherein it switches its function as a holo or apo transferrin receptor leading to either iron delivery or iron export respectively.

Ovotransferrin (conalbumin) is a glycoprotein of egg white albumen. Egg white albumen is composed of multiple proteins, of which ovotransferrin is the most heat reliable. It has a molecular weight of 76,000 daltons and contains about 700 amino acids. Ovotransferrin makes up approximately 13% of egg albumen. As a member of the transferrin and metalloproteinase family, ovotransferrin has been found to possess antibacterial and antioxydant and immunomodulatory properties, arising primarily through its iron (Fe3+) binding capacity by locking away a key biochemical component necessary for micro-organismal survival. Bacteria starved of iron are rendered incapable of moving, making ovotransferrin a potent bacteriostatic.

The iron-responsive element-binding proteins, also known as IRE-BP, IRBP, IRP and IFR , bind to iron-responsive elements (IREs) in the regulation of human iron metabolism.

Iron is an important biological element. It is used in both the ubiquitous iron-sulfur proteins and in vertebrates it is used in hemoglobin which is essential for blood and oxygen transport.

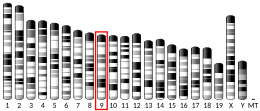
Transferrin receptor 2 (TfR2) is a protein that in humans is encoded by the TFR2 gene. This protein is involved in the uptake of transferrin-bound iron into cells by endocytosis, although its role is minor compared to transferrin receptor 1.

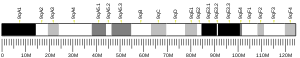
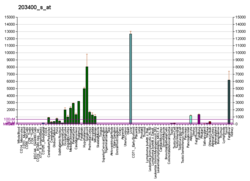
Transferrin receptor protein 1 (TfR1), also known as Cluster of Differentiation 71 (CD71), is a protein that in humans is encoded by the TFRC gene. TfR1 is required for iron import from transferrin into cells by endocytosis.
Haemochromatosis type 3 is a type of iron overload disorder associated with deficiencies in transferrin receptor 2. It exhibits an autosomal recessive inheritance pattern. The first confirmed case was diagnosed in 1865 by French doctor Trousseau. Later in 1889, the German doctor von Recklinghausen indicated that the liver contains iron, and due to bleeding being considered to be the cause, he called the pigment "Haemochromatosis." In 1935, English doctor Sheldon's groundbreaking book titled, Haemochromatosis, reviewed 311 patient case reports and presented the idea that haemochromatosis was a congenital metabolic disorder. Hereditary haemochromatosis is a congenital disorder which affects the regulation of iron metabolism thus causing increased gut absorption of iron and a gradual build-up of pathologic iron deposits in the liver and other internal organs, joint capsules and the skin. The iron overload could potentially cause serious disease from the age of 40–50 years. In the final stages of the disease, the major symptoms include liver cirrhosis, diabetes and bronze-colored skin. There are four types of hereditary hemochromatosis which are classified depending on the age of onset and other factors such as genetic cause and mode of inheritance.
Soluble transferrin receptor conventionally refers to the cleaved extracellular portion of transferrin receptor 1 that is released into serum. This receptor is a protein dimer of two identical subunits, linked together by two pairs of disulfide bonds. Its molecular mass 190,000 Dalton.
Clement Alfred Finch was an American physician specializing in hematology whose research on iron metabolism in the bloodstream at the University of Washington led to significant advancements in accurately diagnosing and treating anemia during a time period in which little was known about this aspect of the body. Finch was distinctively noted for using himself as a test subject by taking blood and bone marrow from his own bones before conducting similar tests on patients. He graduated in 1941 from the University of Rochester Medical School and a year later was married to the first of three wives. He experienced a 60-year tenure at the University of Washington, and has published many scholarly articles pertaining to iron in the bloodstream and is the author of three books entitled: Iron Metabolism (1962), Red Cell Manual (1969) and Fulfilling the Dream: A History of the University of Washington School of Medicine 1946 to 1988 (1990). Finch was elected as a Fellow of the National Academy of Sciences in 1974, and elected as a Fellow of the American Academy of Arts and Sciences in 1976.

KP1019, or indazole trans-[tetrachlorobis(1H-indazole)ruthenate(III)], is one of four ruthenium anti-cancer drugs to enter into phase I clinical trials, the others being BOLD-100, NAMI-A and TLD-1433. Research into ruthenium-based drugs has provided novel alternatives for platinum-based chemotherapeutics such as Cisplatin and its derivatives. KP1019 is useful for metastatic tumors and cis-platin resistant tumors. It exhibits potent cytotoxicity against primary tumors, particularly in colorectal cancer.
Hemochromatosis type 4 is a hereditary iron overload disorder that affects ferroportin, an iron transport protein needed to export iron from cells into circulation. Although the disease is rare, it is found throughout the world and affects people from various ethnic groups. While the majority of individuals with type 4 hemochromatosis have a relatively mild form of the disease, some affected individuals have a more severe form. As the disease progresses, iron may accumulate in the tissues of affected individuals over time, potentially resulting in organ damage.