Dementia is a syndrome associated with many neurodegenerative diseases, characterized by a general decline in cognitive abilities that affects a person's ability to perform everyday activities. This typically involves problems with memory, thinking, behavior, and motor control. Aside from memory impairment and a disruption in thought patterns, the most common symptoms of dementia include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, their caregivers, and their social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than might be caused by the normal aging process.

Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia, rigidity, and postural instability. Both hypokinetic as well as hyperkinetic features are displayed by Parkinsonism.These are the four motor symptoms found in Parkinson's disease (PD) – after which it is named – dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
Hereditary spastic paraplegia (HSP) is a group of inherited diseases whose main feature is a progressive gait disorder. The disease presents with progressive stiffness (spasticity) and contraction in the lower limbs. HSP is also known as hereditary spastic paraparesis, familial spastic paraplegia, French settlement disease, Strumpell disease, or Strumpell-Lorrain disease. The symptoms are a result of dysfunction of long axons in the spinal cord. The affected cells are the primary motor neurons; therefore, the disease is an upper motor neuron disease. HSP is not a form of cerebral palsy even though it physically may appear and behave much the same as spastic diplegia. The origin of HSP is different from cerebral palsy. Despite this, some of the same anti-spasticity medications used in spastic cerebral palsy are sometimes used to treat HSP symptoms.

Donepezil, sold under the brand name Aricept among others, is a medication used to treat dementia of the Alzheimer's type. It appears to result in a small benefit in mental function and ability to function. Use, however, has not been shown to change the progression of the disease. Treatment should be stopped if no benefit is seen. It is taken by mouth or via a transdermal patch.
In physiology, medicine, and anatomy, muscle tone is the continuous and passive partial contraction of the muscles, or the muscle's resistance to passive stretch during resting state. It helps to maintain posture and declines during REM sleep. Muscle tone is regulated by the activity of the motor neurons and can be affected by various factors, including age, disease, and nerve damage.
Hypertonia is a term sometimes used synonymously with spasticity and rigidity in the literature surrounding damage to the central nervous system, namely upper motor neuron lesions. Impaired ability of damaged motor neurons to regulate descending pathways gives rise to disordered spinal reflexes, increased excitability of muscle spindles, and decreased synaptic inhibition. These consequences result in abnormally increased muscle tone of symptomatic muscles. Some authors suggest that the current definition for spasticity, the velocity-dependent over-activity of the stretch reflex, is not sufficient as it fails to take into account patients exhibiting increased muscle tone in the absence of stretch reflex over-activity. They instead suggest that "reversible hypertonia" is more appropriate and represents a treatable condition that is responsive to various therapy modalities like drug or physical therapy.

In pathology, a contracture is a shortening of muscles, tendons, skin, and nearby soft tissues that causes the joints to shorten and become very stiff, preventing normal movement. A contracture is usually permanent, but less commonly can be temporary, or resolve over time but reoccur later in life.
A selective dorsal rhizotomy (SDR), also known as a rhizotomy, dorsal rhizotomy, or a selective posterior rhizotomy, is a neurosurgical procedure that selectively cuts problematic nerve roots in the spinal cord. This procedure has been well-established in the literature as a surgical intervention and is used to relieve negative symptoms of neuromuscular conditions such as spastic diplegia and other forms of spastic cerebral palsy. The specific sensory nerves inducing spasticity are identified using electromyographic (EMG) stimulation and graded on a scale of 1 (mild) to 4. Abnormal nerve responses are isolated and cut, thereby reducing symptoms of spasticity.
Geriatric psychiatry, also known as geropsychiatry, psychogeriatrics or psychiatry of old age, is a branch of medicine and a subspecialty of psychiatry dealing with the study, prevention, and treatment of neurodegenerative, cognitive impairment, and mental disorders in people of old age. Geriatric psychiatry as a subspecialty has significant overlap with the specialties of geriatric medicine, behavioural neurology, neuropsychiatry, neurology, and general psychiatry. Geriatric psychiatry has become an official subspecialty of psychiatry with a defined curriculum of study and core competencies.

Posterior cortical atrophy (PCA), also called Benson's syndrome, is a rare form of dementia which is considered a visual variant or an atypical variant of Alzheimer's disease (AD). The disease causes atrophy of the posterior part of the cerebral cortex, resulting in the progressive disruption of complex visual processing. PCA was first described by D. Frank Benson in 1988.

Central nervous system diseases or central nervous system disorders are a group of neurological disorders that affect the structure or function of the brain or spinal cord, which collectively form the central nervous system (CNS). These disorders may be caused by such things as infection, injury, blood clots, age related degeneration, cancer, autoimmune disfunction, and birth defects. The symptoms vary widely, as do the treatments.
The applause sign is a behavioural indicator, relevant to neurodegenerative conditions, characterised by a patient’s inability to execute the same number of hand claps as demonstrated by an examiner.

Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms. Non-motor symptoms, which include dysautonomia, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common. When other diseases mimic Parkinson's disease, they are categorized as parkinsonism.
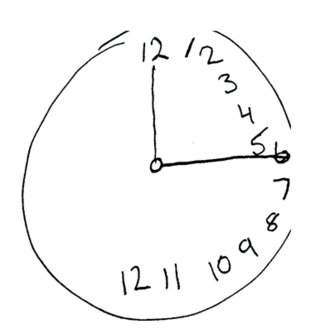
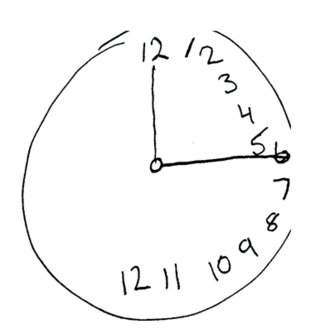
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Clinical Electrophysiological Testing is based on techniques derived from electrophysiology used for the clinical diagnosis of patients. There are many processes that occur in the body which produce electrical signals that can be detected. Depending on the location and the source of these signals, distinct methods and techniques have been developed to properly target them.
The Addenbrooke's Cognitive Examination (ACE) and its subsequent versions are neuropsychological tests used to identify cognitive impairment in conditions such as dementia.
The Self-administered Gerocognitive Examination is a brief cognitive assessment instrument for mild cognitive impairment (MCI) and early dementia, created by Douglas Scharre, Professor of Clinical Neurology and Psychiatry at Ohio State University Wexner Medical Center in Columbus, Ohio.
Jiska Cohen-Mansfield is the Igor Orenstein Chair for the Study of Geriatrics at Tel Aviv University Medical School and a professor at the Department of Health Promotion at the School of Public Health in the Sackler Medical Faculty at Tel Aviv University. She is the director of the Minerva Center for Interdisciplinary Study of End of Life at Tel-Aviv University.

Gladys Elena Maestre is a neuroscientist from Venezuela who is a professor at the University of Texas Rio Grande Valley School of Medicine. She is known for her work on Alzheimer's disease and other forms of dementia.