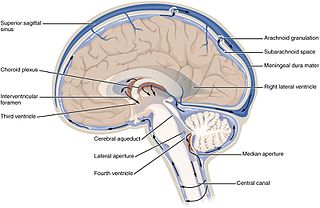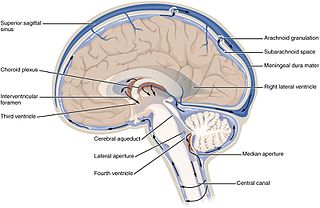
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

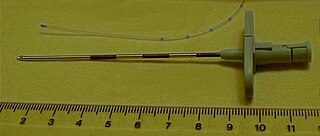
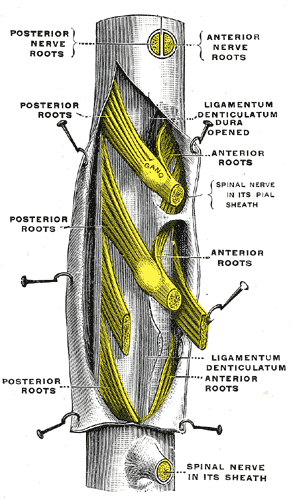
Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.
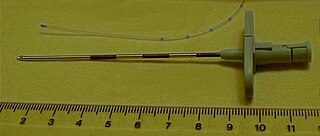
A Tuohy (/tOO-ee/) needle is a hollow hypodermic needle, very slightly curved at the end, suitable for inserting epidural catheters.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

In anatomy, the epidural space is the potential space between the dura mater and vertebrae (spine).

Arachnoiditis is an inflammatory condition of the arachnoid mater or 'arachnoid', one of the membranes known as meninges that surround and protect the central nervous system. The outermost layer of the meninges is the dura mater and adheres to inner surface of the skull and vertebrae. The arachnoid is under or "deep" to the dura and is a thin membrane that adheres directly to the surface of the brain and spinal cord.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

Myelography is a type of radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors. Historically the procedure involved the injection of a radiocontrast agent into the cervical or lumbar spine, followed by several X-ray projections. Today, myelography has largely been replaced by the use of MRI scans, although the technique is still sometimes used under certain circumstances – though now usually in conjunction with CT rather than X-ray projections.

An epidural blood patch (EBP) is a surgical procedure that uses autologous blood, meaning the patient's own blood, in order to close one or many holes in the dura mater of the spinal cord, which occurred as a complication of a lumbar puncture or epidural placement. The punctured dura causes cerebrospinal fluid leak. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH).

Orthostatic headache is a medical condition in which a person develops a headache while vertical and the headache is relieved when horizontal. Previously it was often misdiagnosed as different primary headache disorders such as migraine or tension headaches. Increasing awareness of the symptom and its causes has prevented delayed or missed diagnosis.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord leaks out of one or more holes or tears in the dura mater. A CSF leak is classed as either nonspontaneous (primary), having a known cause, or spontaneous (secondary) where the cause is not readily evident. Causes of a primary CSF leak are those of trauma including from an accident or intentional injury, or arising from a medical intervention known as iatrogenic. A basilar skull fracture as a cause can give the sign of CSF leakage from the ear nose or mouth. A lumbar puncture can give the symptom of a post-dural-puncture headache.
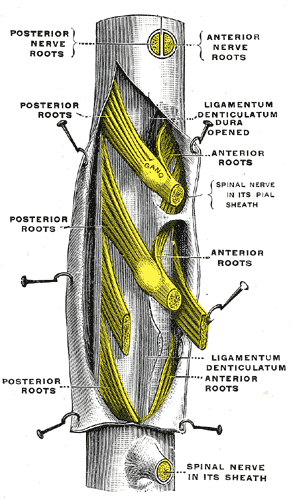
The thecal sac or dural sac is the membranous sheath (theca) or tube of dura mater that surrounds the spinal cord and the cauda equina. The thecal sac contains the cerebrospinal fluid which provides nutrients and buoyancy to the spinal cord. From the skull the tube adheres to bone at the foramen magnum and extends down to the second sacral vertebra where it tapers to cover over the filum terminale. Along most of the spinal canal it is separated from the inner surface by the epidural space. The sac has projections that follow the spinal nerves along their paths out of the vertebral canal which become the dural root sheaths.
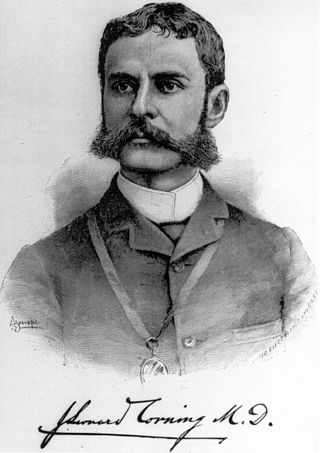
The history of neuraxial anaesthesia dates back to the late 1800s and is closely intertwined with the development of anaesthesia in general. Neuraxial anaesthesia, in particular, is a form of regional analgesia placed in or around the Central Nervous System, used for pain management and anaesthesia for certain surgeries and procedures.
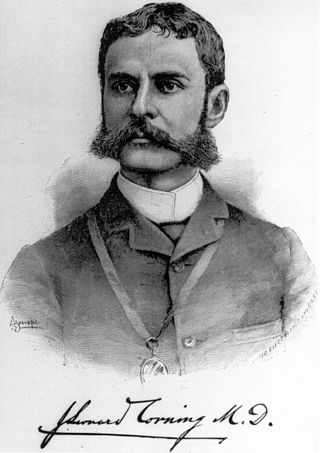
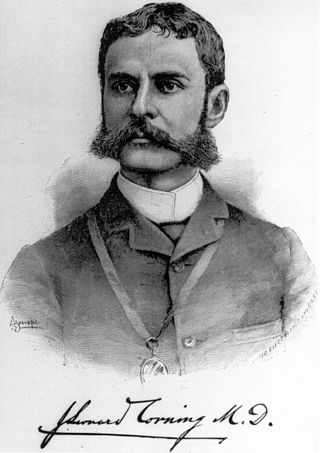
James Leonard Corning was an American neurologist, mainly known for his early experiments on neuraxial blockade in New York City.
Obstetric anesthesia or obstetric anesthesiology, also known as ob-gyn anesthesia or ob-gyn anesthesiology, is a sub-specialty of anesthesiology that provides peripartum pain relief (analgesia) for labor and anesthesia for cesarean deliveries ('C-sections').

Pain management during childbirth is the treatment or prevention of pain that a woman may experience during labor and delivery. The amount of pain a woman feels during labor depends partly on the size and position of her baby, the size of her pelvis, her emotions, the strength of the contractions, and her outlook. Tension increases pain during labor. Virtually all women worry about how they will cope with the pain of labor and delivery. Childbirth is different for each woman and predicting the amount of pain experienced during birth and delivery can not be certain.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.