Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.
Bloodstream infections (BSIs) are infections of blood caused by blood-borne pathogens. The detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is characterized by severe inflammatory or immune responses of the host organism to pathogens.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.
Bronchiolitis is inflammation of the small airways in the lungs. Acute bronchiolitis is due to a viral infection usually affecting children younger than two years of age. Symptoms may include fever, cough, runny nose, wheezing, and breathing problems. More severe cases may be associated with nasal flaring, grunting, or the skin between the ribs pulling in with breathing. If the child has not been able to feed properly, signs of dehydration may be present.

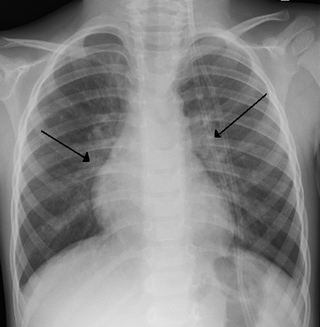
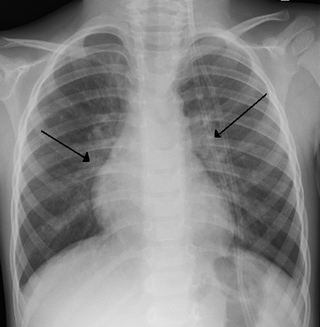
Lower respiratory tract infection (LRTI) is a term often used as a synonym for pneumonia but can also be applied to other types of infection including lung abscess and acute bronchitis. Symptoms include shortness of breath, weakness, fever, coughing and fatigue. A routine chest X-ray is not always necessary for people who have symptoms of a lower respiratory tract infection.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; heavy alcohol use; systemic disease; trauma; and, in children, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis and/or pancreatic failure.

Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.

Carbapenems are a class of very effective antibiotic agents most commonly used for treatment of severe bacterial infections. This class of antibiotics is usually reserved for known or suspected multidrug-resistant (MDR) bacterial infections. Similar to penicillins and cephalosporins, carbapenems are members of the beta-lactam antibiotics drug class, which kill bacteria by binding to penicillin-binding proteins, thus inhibiting bacterial cell wall synthesis. However, these agents individually exhibit a broader spectrum of activity compared to most cephalosporins and penicillins. Furthermore, carbapenems are typically unaffected by emerging antibiotic resistance, even to other beta-lactams.

Norfloxacin, sold under the brand name Noroxin among others, is an antibiotic that belongs to the class of fluoroquinolone antibiotics. It is used to treat urinary tract infections, gynecological infections, inflammation of the prostate gland, gonorrhea and bladder infection. Eye drops were approved for use in children older than one year of age.
Ventilator-associated pneumonia (VAP) is a type of lung infection that occurs in people who are on mechanical ventilation breathing machines in hospitals. As such, VAP typically affects critically ill persons that are in an intensive care unit (ICU) and have been on a mechanical ventilator for at least 48 hours. VAP is a major source of increased illness and death. Persons with VAP have increased lengths of ICU hospitalization and have up to a 20–30% death rate. The diagnosis of VAP varies among hospitals and providers but usually requires a new infiltrate on chest x-ray plus two or more other factors. These factors include temperatures of >38 °C or <36 °C, a white blood cell count of >12 × 109/ml, purulent secretions from the airways in the lung, and/or reduction in gas exchange.

Respiratory tract infections (RTIs) are infectious diseases involving the lower or upper respiratory tract. An infection of this type usually is further classified as an upper respiratory tract infection or a lower respiratory tract infection. Lower respiratory infections, such as pneumonia, tend to be far more severe than upper respiratory infections, such as the common cold.

Meningococcal disease describes infections caused by the bacterium Neisseria meningitidis. It has a high mortality rate if untreated but is vaccine-preventable. While best known as a cause of meningitis, it can also result in sepsis, which is an even more damaging and dangerous condition. Meningitis and meningococcemia are major causes of illness, death, and disability in both developed and under-developed countries.

Eosinopenia is a condition where the number of eosinophils, a type of white blood cell, in circulating blood is lower than normal. Eosinophils are a type of granulocyte and consequently from the same cellular lineage as neutrophils, basophils, and mast cells. Along with the other granulocytes, eosinophils are part of the innate immune system and contribute to the defense of the body from pathogens. The most widely understood function of eosinophils is in association with allergy and parasitic disease processes, though their functions in other pathologies are the subject of ongoing research. The opposite phenomenon, in which the number of eosinophils present in the blood is higher than normal, is known as eosinophilia.
Pneumococcal infection is an infection caused by the bacterium Streptococcus pneumoniae.

Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, intense headache, vomiting and neck stiffness and occasionally photophobia.
Neonatal sepsis is a type of neonatal infection and specifically refers to the presence in a newborn baby of a bacterial blood stream infection (BSI) in the setting of fever. Older textbooks may refer to neonatal sepsis as "sepsis neonatorum". Criteria with regards to hemodynamic compromise or respiratory failure are not useful clinically because these symptoms often do not arise in neonates until death is imminent and unpreventable. Neonatal sepsis is divided into two categories: early-onset sepsis (EOS) and late-onset sepsis (LOS). EOS refers to sepsis presenting in the first 7 days of life, with LOS referring to presentation of sepsis after 7 days. Neonatal sepsis is the single most common cause of neonatal death in hospital as well as community in developing country.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.
Enitan Carrol is a British physician and Professor of Clinical Infection, Microbiology and Immunology. Carrol studies the mechanisms that underpin bacterial infection. In 2020 she was featured in Nicola Rollock's exhibition Phenomenal Women: Portraits of UK Black Female Professors.
Presepsin is a 13-kDa-cleavage product of CD14 receptor.