Ultraviolet (UV) is a form of electromagnetic radiation with wavelength shorter than that of visible light, but longer than X-rays. UV radiation is present in sunlight, and constitutes about 10% of the total electromagnetic radiation output from the Sun. It is also produced by electric arcs; Cherenkov radiation; and specialized lights; such as mercury-vapor lamps, tanning lamps, and black lights. Although long-wavelength ultraviolet is not considered an ionizing radiation because its photons lack the energy to ionize atoms, it can cause chemical reactions and causes many substances to glow or fluoresce. Many practical applications, including chemical and biological effects, derive from the way that UV radiation can interact with organic molecules. These interactions can involve absorption or adjusting energy states in molecules, but do not necessarily involve heating.

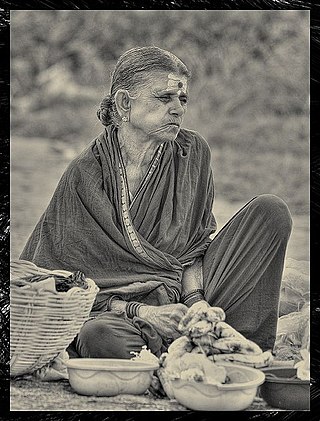
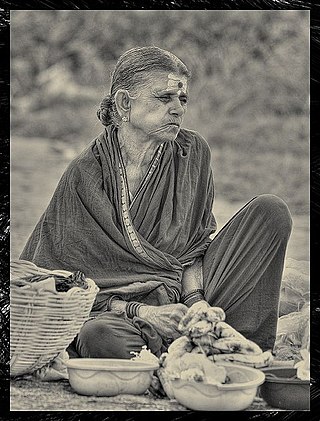
Vitiligo is a chronic autoimmune disorder that causes patches of skin to lose pigment or color. The cause of vitiligo is unknown, but it may be related to immune system changes, genetic factors, stress, or sun exposure. Treatment options include topical medications, light therapy, surgery and cosmetics.
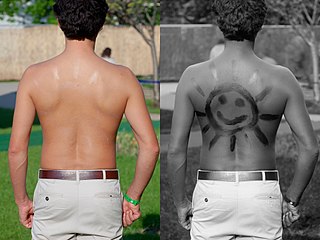
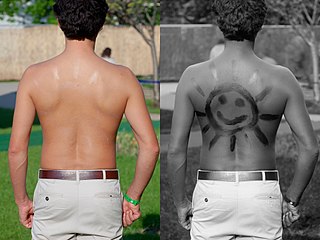
Sunscreen, also known as sunblock or sun cream, is a photoprotective topical product for the skin that helps protect against sunburn and most importantly prevent skin cancer. Sunscreens come as lotions, sprays, gels, foams, sticks, powders and other topical products. Sunscreens are common supplements to clothing, particularly sunglasses, sunhats and special sun protective clothing, and other forms of photoprotection.

A blacklight, also called a UV-A light, Wood's lamp, or ultraviolet light, is a lamp that emits long-wave (UV-A) ultraviolet light and very little visible light. One type of lamp has a violet filter material, either on the bulb or in a separate glass filter in the lamp housing, which blocks most visible light and allows through UV, so the lamp has a dim violet glow when operating. Blacklight lamps which have this filter have a lighting industry designation that includes the letters "BLB". This stands for "blacklight blue". A second type of lamp produces ultraviolet but does not have the filter material, so it produces more visible light and has a blue color when operating. These tubes are made for use in "bug zapper" insect traps, and are identified by the industry designation "BL". This stands for "blacklight".

Indoor tanning involves using a device that emits ultraviolet radiation to produce a cosmetic tan. Typically found in tanning salons, gyms, spas, hotels, and sporting facilities, and less often in private residences, the most common device is a horizontal tanning bed, also known as a sunbed or solarium. Vertical devices are known as tanning booths or stand-up sunbeds.

Contact dermatitis is a type of acute or chronic inflammation of the skin caused by exposure to chemical or physical agents. Symptoms of contact dermatitis can include itchy or dry skin, a red rash, bumps, blisters, or swelling. These rashes are not contagious or life-threatening, but can be very uncomfortable.

Light therapy, also called phototherapy or bright light therapy is the exposure to direct sunlight or artificial light at controlled wavelengths in order to treat a variety of medical disorders, including seasonal affective disorder (SAD), circadian rhythm sleep-wake disorders, cancers, and skin wound infections. Treating skin conditions such as neurodermatitis, psoriasis, acne vulgaris, and eczema with ultraviolet light is called ultraviolet light therapy.

Hives, also known as urticaria, is a kind of skin rash with red, raised, itchy bumps. Hives may burn or sting. The patches of rash may appear on different body parts, with variable duration from minutes to days, and does not leave any long-lasting skin change. Fewer than 5% of cases last for more than six weeks. The condition frequently recurs.

Ultraviolet light therapy or ultraviolet phototherapy is a treatment for psoriasis, atopic skin disorder, vitiligo and other skin diseases.

Cold urticaria is a disorder in which large red welts called hives (urticaria) form on the skin after exposure to a cold stimulus. The hives are usually itchy and often the hands and feet will become itchy and swollen as well. Hives vary in size from about 7 mm in diameter to as big as about 27 mm or larger.
PUVA is an ultraviolet light therapy treatment for skin diseases: vitiligo, eczema, psoriasis, graft-versus-host disease, mycosis fungoides, large plaque parapsoriasis, and cutaneous T-cell lymphoma, using the sensitizing effects of the drug psoralen. The psoralen is applied or taken orally to sensitize the skin, then the skin is exposed to UVA.
Light sensitivity or photosensitivity refers to a notable or increased reactivity to light. Apart from vision, human beings have many physiological and psychological responses to light. In rare individuals an atypical response may result in serious discomfort, disease, or injury. Some drugs have a photosensitizing effect. Properties of natural or artificial light that may abnormally affect people include:
Photodermatoses is a skin condition resulting in abnormal skin reactions to ultraviolet (UV) radiation. These abnormal skin reactions may develop into rashes. While reactions to UV radiation is common, true photodermatoses is considered when an abnormal reaction is caused by UV-A rays or radiation between 320–400 nm.

Polymorphous light eruption (PLE) presents with itchy red small bumps on sun-exposed skin, particularly face, neck, forearms and legs. It generally appears 30 minutes to a few hours after sun exposure and may last between one and 14 days. The bumps may become small blisters or plaques and may appear bloody,often healing with minimal scarring.
Actinic prurigo is a rare sunlight-induced, pruritic, papular, or nodular skin eruption. Some medical experts use the term actinic prurigo to denote a rare photodermatosis that develops in childhood and is chronic and persistent; this rare photodermatosis, associated with the human leukocyte antigen HLA-DR4, is often called "Familial polymorphous light eruption of American Indians" or "Hereditary polymorphous light eruption of American Indians" but some experts consider it to be a variant of the syndrome known as polymorphous light eruption (PMLE). Some experts use the term actinic prurigo for Hutchinson's summer prurigo and several other photodermatoses that might, or might not, be distinct clinical entities.

Sunburn is a form of radiation burn that affects living tissue, such as skin, that results from an overexposure to ultraviolet (UV) radiation, usually from the Sun. Common symptoms in humans and other animals include red or reddish skin that is hot to the touch or painful, general fatigue, and mild dizziness. Other symptoms include blistering, peeling skin, swelling, itching, and nausea. Excessive UV radiation is the leading cause of (primarily) non-malignant skin tumors, which in extreme cases can be life-threatening. Sunburn is an inflammatory response in the tissue triggered by direct DNA damage by UV radiation. When the cells' DNA is overly damaged by UV radiation, type I cell-death is triggered and the tissue is replaced.
Acne aestivalis also called as acne mallorca, is a special kind of polymorphous light eruption induced by ultra violet A radiation. This condition is said to be seasonal, usually affecting people in springtime and goes away in autumn when there is less sun light. This photo induced skin reaction leads to a mono-morphous eruption that consists of multiple, uniform, red, papular lesions. This skin reaction is classified as a delayed-type hypersensitivity because the onset is 24–72 hours after sun exposure. The condition equally affects men and women between the ages of 20–40 years old with no prior history of acne vulgaris. The eruption is unusual because it spares the face but it affects the lateral aspects of the upper arms, shoulder girdle, back, and chest. This condition's pathogenesis is not very well understood but scientists believe it an unfortunate side effect that results from a strong immune response to potentially cancer-causing cell damage.
Photoaging or photoageing is a term used for the characteristic changes to skin induced by chronic UVA and UVB exposure. Tretinoin is the best studied retinoid in the treatment of photoaging.

Exposing skin to the ultraviolet radiation in sunlight has both positive and negative health effects. On the positive side, exposure allows for the synthesis of vitamin D3. Vitamin D has been suggested as having a wide range of positive health effects, which include strengthening bones and possibly inhibiting the growth of some cancers. A dietary supplement can also supply vitamin D, but there are also benefits to exposure not obtainable through Vitamin D supplementation. Long-term sun exposure is associated with reduced all-cause mortality and reduced mortality risk from cardiovascular disease (CVD), some forms of cancer, and non-CVD/noncancer related disease, with indications in these studies that Vitamin D is not the mediator. Supplementation offers limited bioavailability and no synthesis of subdermal nitric oxide. UV exposure also has positive effects for endorphin levels, and possibly for protection against multiple sclerosis. Abundant visible light to the eyes gives health benefits through its association with the timing of melatonin synthesis, maintenance of normal and robust circadian rhythms, and reduced risk of seasonal affective disorder.
Bernadette Eberlein is a dermatologist, allergologist, academic, and researcher. She is the Senior Physician of the private outpatient clinic, the Photodermatology unit, the unit for Soft X-Ray Therapy at Technical University of Munich.