Personal protective equipment (PPE) is protective clothing, helmets, goggles, or other garments or equipment designed to protect the wearer's body from injury or infection. The hazards addressed by protective equipment include physical, electrical, heat, chemical, biohazards, and airborne particulate matter. Protective equipment may be worn for job-related occupational safety and health purposes, as well as for sports and other recreational activities. Protective clothing is applied to traditional categories of clothing, and protective gear applies to items such as pads, guards, shields, or masks, and others. PPE suits can be similar in appearance to a cleanroom suit.
In medicine, public health, and biology, transmission is the passing of a pathogen causing communicable disease from an infected host individual or group to a particular individual or group, regardless of whether the other individual was previously infected. The term strictly refers to the transmission of microorganisms directly from one individual to another by one or more of the following means:

A surgical mask, also known by other names such as a medical face mask or procedure mask, is a personal protective equipment used by healthcare professionals that serves as a mechanical barrier that interferes with direct airflow in and out of respiratory orifices. This helps reduce airborne transmission of pathogens and other aerosolized contaminants between the wearer and nearby people via respiratory droplets ejected when sneezing, coughing, forceful expiration or unintentionally spitting when talking, etc. Surgical masks may be labeled as surgical, isolation, dental or medical procedure masks.

A respirator is a device designed to protect the wearer from inhaling hazardous atmospheres including fumes, vapours, gases and particulate matter such as dusts and airborne pathogens such as viruses. There are two main categories of respirators: the air-purifying respirator, in which respirable air is obtained by filtering a contaminated atmosphere, and the air-supplied respirator, in which an alternate supply of breathable air is delivered. Within each category, different techniques are employed to reduce or eliminate noxious airborne contaminants.

Respiratory tract infections (RTIs) are infectious diseases involving the lower or upper respiratory tract. An infection of this type usually is further classified as an upper respiratory tract infection or a lower respiratory tract infection. Lower respiratory infections, such as pneumonia, tend to be far more severe than upper respiratory infections, such as the common cold.

In health care facilities, isolation represents one of several measures that can be taken to implement in infection control: the prevention of communicable diseases from being transmitted from a patient to other patients, health care workers, and visitors, or from outsiders to a particular patient. Various forms of isolation exist, in some of which contact procedures are modified, and others in which the patient is kept away from all other people. In a system devised, and periodically revised, by the U.S. Centers for Disease Control and Prevention (CDC), various levels of patient isolation comprise application of one or more formally described "precaution".

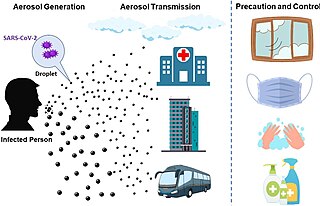
Airborne transmission or aerosol transmission is transmission of an infectious disease through small particles suspended in the air. Infectious diseases capable of airborne transmission include many of considerable importance both in human and veterinary medicine. The relevant infectious agent may be viruses, bacteria, or fungi, and they may be spread through breathing, talking, coughing, sneezing, raising of dust, spraying of liquids, flushing toilets, or any activities which generate aerosol particles or droplets. This is the transmission of diseases via transmission of an infectious agent, and does not include diseases caused by air pollution.
Influenza prevention involves taking steps that one can use to decrease their chances of contracting flu viruses, such as the Pandemic H1N1/09 virus, responsible for the 2009 flu pandemic.
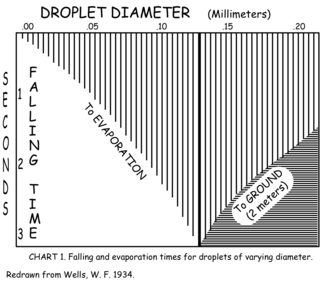
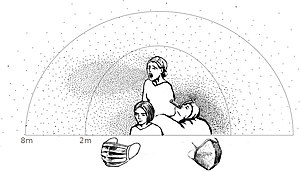
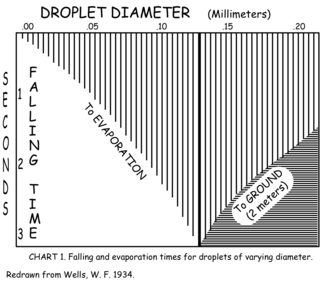
The Wells curve is a diagram, developed by W. F. Wells in 1934, which describes what is expected to happen to small droplets once they have been exhaled into air. Coughing, sneezing, and other violent exhalations produce high numbers of respiratory droplets derived from saliva and/or respiratory mucus, with sizes ranging from about 1 µm to 2 mm. Wells' insight was that such droplets would have two distinct fates, depending on their sizes. The interplay of gravity and evaporation means that droplets larger than a humidity-determined threshold size would fall to the ground due to gravity, while droplets smaller than this size would quickly evaporate, leaving a dry residue that drifts in the air. Since droplets from an infected person may contain infectious bacteria or viruses, these processes influence transmission of respiratory diseases.
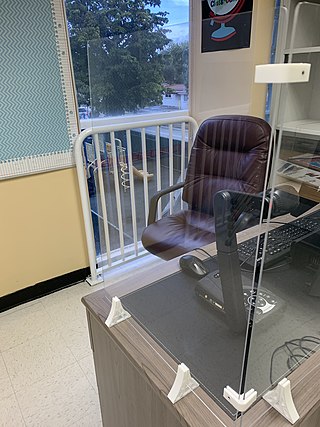
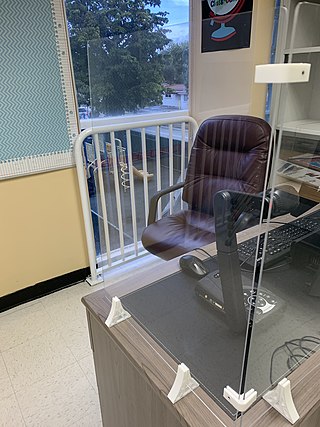
A sneeze guard, sneezeguard, or cough shield is an acrylic or glass screen designed to protect food or people from the exposure to respiratory droplets, which are dispensed when coughing, sneezing, or speaking. Sneeze guards have been in use in restaurants for decades. With the rise of the COVID-19 pandemic, sneeze guards have been installed in public places like offices, schools and retail stores to reduce the risk of infection through respiratory droplets.

A respiratory droplet is a small aqueous droplet produced by exhalation, consisting of saliva or mucus and other matter derived from respiratory tract surfaces. Respiratory droplets are produced naturally as a result of breathing, speaking, sneezing, coughing, or vomiting, so they are always present in our breath, but speaking and coughing increase their number.

An N95 filtering facepiece respirator, commonly abbreviated N95 respirator, is a particulate-filtering facepiece respirator that meets the U.S. National Institute for Occupational Safety and Health (NIOSH) N95 classification of air filtration, meaning that it filters at least 95% of airborne particles that have a mass median aerodynamic diameter of 0.3 micrometers. This standard does not require that the respirator be resistant to oil; another standard, P95, adds that requirement. The N95 type is the most common particulate-filtering facepiece respirator. It is an example of a mechanical filter respirator, which provides protection against particulates but not against gases or vapors. An authentic N95 respirator is marked with the text "NIOSH" or the NIOSH logo, the filter class ("N95"), a "TC" approval number of the form XXX-XXXX, the approval number must be listed on the NIOSH Certified Equipment List (CEL) or the NIOSH Trusted-Source page, and it must have headbands instead of ear loops.

Hazard controls for COVID-19 in workplaces are the application of occupational safety and health methodologies for hazard controls to the prevention of COVID-19. Vaccination is the most effective way to protect against severe illness or death from COVID-19. Multiple layers of controls are recommended, including measures such as remote work and flextime, increased ventilation, personal protective equipment (PPE) and face coverings, social distancing, and enhanced cleaning programs.

A cloth face mask is a mask made of common textiles, usually cotton, worn over the mouth and nose. When more effective masks are not available, and when physical distancing is impossible, cloth face masks are recommended by public health agencies for disease "source control" in epidemic situations to protect others from virus laden droplets in infected mask wearers' breath, coughs, and sneezes. Because they are less effective than N95 masks, surgical masks, or physical distancing in protecting the wearer against viruses, they are not considered to be personal protective equipment by public health agencies. They are used by the general public in household and community settings as protection against both infectious diseases and particulate air pollution.

Mechanical filters are a class of filter for air-purifying respirators that mechanically stops particulates from reaching the wearer's nose and mouth. They come in multiple physical forms.

During the COVID-19 pandemic, face masks or coverings, including N95, FFP2, surgical, and cloth masks, have been employed as public and personal health control measures against the spread of SARS-CoV-2, the virus that causes COVID-19.
In epidemiology, a non-pharmacological intervention (NPI) is any method used to reduce the spread of an epidemic disease without requiring pharmacological drug treatments. Examples of non-pharmacological interventions that reduce the spread of infectious diseases include wearing a face mask and staying away from sick people.
The transmission of COVID-19 is the passing of coronavirus disease 2019 from person to person. COVID-19 is mainly transmitted when people breathe in air contaminated by droplets/aerosols and small airborne particles containing the virus. Infected people exhale those particles as they breathe, talk, cough, sneeze, or sing. Transmission is more likely the closer people are. However, infection can occur over longer distances, particularly indoors.
FFP standards refer to the filtering half mask classification by EN 149, a European standard of testing and marking requirements for filtering half masks. FFP standard masks cover the nose, mouth and chin and may have inhalation and/or exhalation valves.
Nicole M. Bouvier is an American physician who is Professor of Medicine at Icahn School of Medicine at Mount Sinai. Her research considers the environmental and viral factors that impact respiratory transmission of influenza viruses.