Related Research Articles

The lungs are the most important organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of the heart. Their function in the respiratory system is to extract oxygen from the air and transfer it into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere, in a process of gas exchange. The pleurae, which are thin, smooth, and moist, serve to reduce friction between the lungs and chest wall during breathing, allowing for easy and effortless movements of the lungs.

In vertebrate anatomy, ribs are the long curved bones which form the rib cage, part of the axial skeleton. In most tetrapods, ribs surround the chest, enabling the lungs to expand and thus facilitate breathing by expanding the chest cavity. They serve to protect the lungs, heart, and other internal organs of the thorax. In some animals, especially snakes, ribs may provide support and protection for the entire body.

The trachea, also known as the windpipe, is a cartilaginous tube that connects the larynx to the bronchi of the lungs, allowing the passage of air, and so is present in almost all animals with lungs. The trachea extends from the larynx and branches into the two primary bronchi. At the top of the trachea the cricoid cartilage attaches it to the larynx. The trachea is formed by a number of horseshoe-shaped rings, joined together vertically by overlying ligaments, and by the trachealis muscle at their ends. The epiglottis closes the opening to the larynx during swallowing.

The esophagus or oesophagus, colloquially known also as the food pipe, food tube, or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.
Tracheomalacia is a condition or incident where the cartilage that keeps the airway (trachea) open is soft such that the trachea partly collapses especially during increased airflow. This condition is most commonly seen in infants and young children. The usual symptom is stridor when a person breathes out. This is usually known as a collapsed windpipe.

The respiratory tract is the subdivision of the respiratory system involved with the process of respiration in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

In human anatomy, the subclavian arteries are paired major arteries of the upper thorax, below the clavicle. They receive blood from the aortic arch. The left subclavian artery supplies blood to the left arm and the right subclavian artery supplies blood to the right arm, with some branches supplying the head and thorax. On the left side of the body, the subclavian comes directly off the aortic arch, while on the right side it arises from the relatively short brachiocephalic artery when it bifurcates into the subclavian and the right common carotid artery.

A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

Vernix caseosa, also known as vernix, is the waxy white substance found coating the skin of newborn human babies. It is produced by dedicated cells and is thought to have some protective roles during fetal development and for a few hours after birth.

The umbilical artery is a paired artery that is found in the abdominal and pelvic regions. In the fetus, it extends into the umbilical cord.

The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles. There are two recurrent laryngeal nerves, right and left. The right and left nerves are not symmetrical, with the left nerve looping under the aortic arch, and the right nerve looping under the right subclavian artery then traveling upwards. They both travel alongside the trachea. Additionally, the nerves are among the few nerves that follow a recurrent course, moving in the opposite direction to the nerve they branch from, a fact from which they gain their name.

The cricothyroid ligament is a ligament in the neck. It connects the cricoid cartilage to the thyroid cartilage. It prevents these cartilages from moving too far apart. It is cut during an emergency cricothyrotomy to treat upper airway obstruction.

The cricothyroid muscle is the only tensor muscle of the larynx aiding with phonation. It is innervated by the superior laryngeal nerve. Its action tilts the thyroid forward to help tense the vocal cords, thus increasing the pitch of the voice.

The aortic arch, arch of the aorta, or transverse aortic arch is the part of the aorta between the ascending and descending aorta. The arch travels backward, so that it ultimately runs to the left of the trachea.

The duodenojejunal flexure or duodenojejunal junction, also known as the angle of Treitz, is the border between the duodenum and the jejunum.

The vitelline veins are veins that drain blood from the yolk sac and the gut tube during gestation.

The carina of trachea is a ridge of cartilage at the base of the trachea separating the openings of the left and right main bronchi.

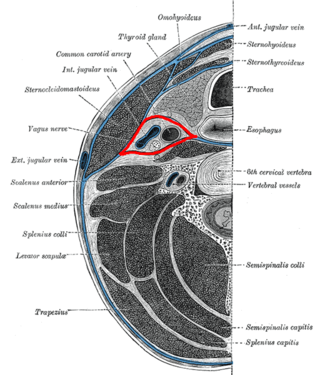
The pretracheal fascia is a layer of the deep cervical fascia at the front of the neck. It attaches to the hyoid bone above, and - extending down into the thorax - blends with the fibrous pericardium below. It encloses the thyroid gland and parathyroid glands, trachea, and esophagus. It extends medially in front of the carotid vessels. It assists in forming the carotid sheath.
The buccopharyngeal fascia is a fascia of the pharynx. It represents the posterior portion of the pretracheal fascia. It covers the superior pharyngeal constrictor muscles, and buccinator muscle.
The tracheoesophageal septum is an embryological structure. It is formed from the tracheoesophageal folds or ridges which fuse in the midline. It divides the oesophagus from the trachea during prenatal development. Developmental abnormalities can lead to a tracheoesophageal fistula.
References
- 1 2 Lumb, Andrew B (2017-01-01), Lumb, Andrew B (ed.), "Chapter 1 - Functional Anatomy of the Respiratory Tract", Nunn's Applied Respiratory Physiology (Eighth Edition), Elsevier, pp. 3–16.e1, ISBN 978-0-7020-6294-0 , retrieved 2021-01-21
- 1 2 Ross, Michael H.; Pawlina, Wojciech (2005), Histology a Text and Atlas (5th edition), LWW, p. 617, ISBN 0781750563
- 1 2 Leslie, Kevin O.; Wick, Mark R. (2018-01-01), Leslie, Kevin O.; Wick, Mark R. (eds.), "1 - Lung Anatomy", Practical Pulmonary Pathology: A Diagnostic Approach (Third Edition), Elsevier, pp. 1–14.e2, ISBN 978-0-323-44284-8 , retrieved 2021-01-23
- ↑ Rosado-de-Christenson, Melissa L.; Carter, Brett W., eds. (2016-01-01), "Approach to Tracheobronchial Neoplasms", Specialty Imaging: Thoracic Neoplasms, Specialty Imaging, Philadelphia: Elsevier, pp. 230–235, doi:10.1016/B978-0-323-37706-5.50069-X, ISBN 978-0-323-37706-5 , retrieved 2021-01-23
- ↑ Shaffer, Thomas H.; Penn, Raymond B.; Wolfson, Marla R. (2017-01-01), Polin, Richard A.; Abman, Steven H.; Rowitch, David H.; Benitz, William E. (eds.), "66 - Upper Airway Structure: Function, Regulation, and Development", Fetal and Neonatal Physiology (Fifth Edition), Elsevier, pp. 676–685.e2, ISBN 978-0-323-35214-7 , retrieved 2021-01-23
- ↑ Wert, Susan E. (2017-01-01), Polin, Richard A.; Abman, Steven H.; Rowitch, David H.; Benitz, William E. (eds.), "61 - Normal and Abnormal Structural Development of the Lung", Fetal and Neonatal Physiology (Fifth Edition), Elsevier, pp. 627–641.e3, ISBN 978-0-323-35214-7 , retrieved 2021-01-23
- ↑ Morgenroth, Konrad; Ebsen, Michael (2008-01-01), Papadakos, PETER J.; Lachmann, BURKHARD; Visser-Isles, Laraine (eds.), "CHAPTER 8 - Anatomy", Mechanical Ventilation, Philadelphia: W.B. Saunders, pp. 69–85, ISBN 978-0-7216-0186-1 , retrieved 2021-01-23
- 1 2 3 Cravero, Joseph P.; Landrigan-Ossar, Mary (2019-01-01), Coté, Charles J.; Lerman, Jerrold; Anderson, Brian J. (eds.), "46 - Anesthesia Outside the Operating Room", A Practice of Anesthesia for Infants and Children (Sixth Edition), Philadelphia: Elsevier, pp. 1077–1094.e4, ISBN 978-0-323-42974-0 , retrieved 2021-01-23