Diabetes insipidus (DI), alternately called arginine vasopressin deficiency (AVP-D) or arginine vasopressin resistance (AVP-R), is a condition characterized by large amounts of dilute urine and increased thirst. The amount of urine produced can be nearly 20 liters per day. Reduction of fluid has little effect on the concentration of the urine. Complications may include dehydration or seizures.

The hypothalamus is a small part of the vertebrate brain that contains a number of nuclei with a variety of functions. One of the most important functions is to link the nervous system to the endocrine system via the pituitary gland. The hypothalamus is located below the thalamus and is part of the limbic system. It forms the basal part of the diencephalon. All vertebrate brains contain a hypothalamus. In humans, it is about the size of an almond.
Hyponatremia or hyponatraemia is a low concentration of sodium in the blood. It is generally defined as a sodium concentration of less than 135 mmol/L (135 mEq/L), with severe hyponatremia being below 120 mEq/L. Symptoms can be absent, mild or severe. Mild symptoms include a decreased ability to think, headaches, nausea, and poor balance. Severe symptoms include confusion, seizures, and coma; death can ensue.

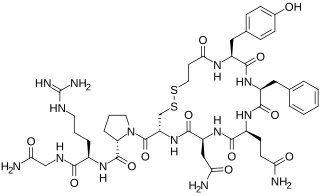
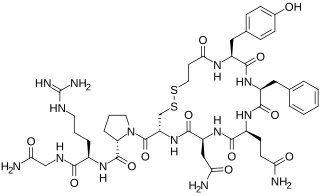
Human vasopressin, also called antidiuretic hormone (ADH), arginine vasopressin (AVP) or argipressin, is a hormone synthesized from the AVP gene as a peptide prohormone in neurons in the hypothalamus, and is converted to AVP. It then travels down the axon terminating in the posterior pituitary, and is released from vesicles into the circulation in response to extracellular fluid hypertonicity (hyperosmolality). AVP has two primary functions. First, it increases the amount of solute-free water reabsorbed back into the circulation from the filtrate in the kidney tubules of the nephrons. Second, AVP constricts arterioles, which increases peripheral vascular resistance and raises arterial blood pressure.

The posterior pituitary is the posterior lobe of the pituitary gland which is part of the endocrine system. The posterior pituitary is not glandular as is the anterior pituitary. Instead, it is largely a collection of axonal projections from the hypothalamus that terminate behind the anterior pituitary, and serve as a site for the secretion of neurohypophysial hormones directly into the blood. The hypothalamic–neurohypophyseal system is composed of the hypothalamus, posterior pituitary, and these axonal projections.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.
Polydipsia is excessive thirst or excess drinking. The word derives from the Greek πολυδίψιος (poludípsios) "very thirsty", which is derived from πολύς + δίψα. Polydipsia is a nonspecific symptom in various medical disorders. It also occurs as an abnormal behaviour in some non-human animals, such as in birds.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.
Desmopressin, sold under the trade name DDAVP among others, is a medication used to treat diabetes insipidus, bedwetting, hemophilia A, von Willebrand disease, and high blood urea levels. In hemophilia A and von Willebrand disease, it should only be used for mild to moderate cases. It may be given in the nose, by injection into a vein, by mouth, or under the tongue.
Hypernatremia, also spelled hypernatraemia, is a high concentration of sodium in the blood. Early symptoms may include a strong feeling of thirst, weakness, nausea, and loss of appetite. Severe symptoms include confusion, muscle twitching, and bleeding in or around the brain. Normal serum sodium levels are 135–145 mmol/L. Hypernatremia is generally defined as a serum sodium level of more than 145 mmol/L. Severe symptoms typically only occur when levels are above 160 mmol/L.
The syndrome of inappropriate antidiuretic hormone secretion (SIADH), also known as the syndrome of inappropriate antidiuresis (SIAD), is characterized by a physiologically inappropriate release of antidiuretic hormone (ADH) either from the posterior pituitary gland, or an abnormal non-pituitary source. Unsuppressed ADH causes a physiologically inappropriate increase in solute-free water being reabsorbed by the tubules of the kidney to the venous circulation leading to hypotonic hyponatremia.

Conivaptan, sold under the brand name Vaprisol, is a non-peptide inhibitor of the receptor for anti-diuretic hormone, also called vasopressin. It was approved in 2004 for hyponatremia. The compound was discovered by Astellas and marked in 2006. The drug is now marketed by Cumberland Pharmaceuticals, Inc.
An osmoreceptor is a sensory receptor primarily found in the hypothalamus of most homeothermic organisms that detects changes in osmotic pressure. Osmoreceptors can be found in several structures, including two of the circumventricular organs – the vascular organ of the lamina terminalis, and the subfornical organ. They contribute to osmoregulation, controlling fluid balance in the body. Osmoreceptors are also found in the kidneys where they also modulate osmolality.
Nephrogenic diabetes insipidus, recently renamed arginine vasopressin resistance (AVP-R) and previously known as renal diabetes insipidus, is a form of diabetes insipidus primarily due to pathology of the kidney. This is in contrast to central or neurogenic diabetes insipidus, which is caused by insufficient levels of vasopressin. Nephrogenic diabetes insipidus is caused by an improper response of the kidney to vasopressin, leading to a decrease in the ability of the kidney to concentrate the urine by removing free water.

Primary polydipsia and psychogenic polydipsia are forms of polydipsia characterised by excessive fluid intake in the absence of physiological stimuli to drink. Psychogenic polydipsia caused by psychiatric disorders—oftentimes schizophrenia—is frequently accompanied by the sensation of dry mouth. Some conditions with polydipsia as a symptom are explicitly non-psychogenic. Primary polydipsia is a diagnosis of exclusion.

A fluid or water deprivation test is a medical test which can be used to determine whether the patient has diabetes insipidus as opposed to other causes of polydipsia. The patient is required, for a prolonged period, to forgo intake of water completely, to determine the cause of the thirst.

Neurophysin II is a carrier protein with a size of 19,687.3 Da and is made up of a dimer of two virtually identical chains of amino acids. Neurophysin II is a cleavage product of the AVP gene. It is a neurohypophysial hormone that is transported in vesicles with vasopressin, the other cleavage product, along axons, from magnocellular neurons of the hypothalamus to the posterior lobe of the pituitary. Although it is stored in neurosecretory granules with vasopressin and released with vasopressin into the bloodstream, its biological action is unclear. Neurophysin II is also known as a stimulator of prolactin secretion.
Central diabetes insipidus, recently renamed arginine vasopressin deficiency (AVP-D), is a form of diabetes insipidus that is due to a lack of vasopressin (ADH) production in the brain. Vasopressin acts to increase the volume of blood (intravascularly), and decrease the volume of urine produced. Therefore, a lack of it causes increased urine production and volume depletion.
Hypothalamic disease is a disorder presenting primarily in the hypothalamus, which may be caused by damage resulting from malnutrition, including anorexia and bulimia eating disorders, genetic disorders, radiation, surgery, head trauma, lesion, tumour or other physical injury to the hypothalamus. The hypothalamus is the control center for several endocrine functions. Endocrine systems controlled by the hypothalamus are regulated by antidiuretic hormone (ADH), corticotropin-releasing hormone, gonadotropin-releasing hormone, growth hormone-releasing hormone, oxytocin, all of which are secreted by the hypothalamus. Damage to the hypothalamus may impact any of these hormones and the related endocrine systems. Many of these hypothalamic hormones act on the pituitary gland. Hypothalamic disease therefore affects the functioning of the pituitary and the target organs controlled by the pituitary, including the adrenal glands, ovaries and testes, and the thyroid gland.
Copeptin is a 39-amino acid-long peptide derived from the C-terminus of pre-pro-hormone of arginine vasopressin, neurophysin II and copeptin. Arginine vasopressin (AVP), also known as the antidiuretic hormone (ADH), is encoded by the AVP gene and is involved in multiple cardiovascular and renal pathways and abnormal level of AVP are associated with various diseases. Hence measurement of AVP would be useful, but is not commonly carried out in clinical practice because of its very short half-life making it difficult to quantify. In contrast, copeptin can be immunologically tested with ease and therefore can be used as a vasopressin surrogate marker.