Health informatics is the study and implementation of computer structures and algorithms to improve communication, understanding, and management of medical information. It can be viewed as branch of engineering and applied science.

The Sociedade Brasileira de Informática em Saúde, abbreviated as SBIS, is a professional society created in November 1986 in Campinas, during the First Brazilian Congress on Health Informatics. It has the mission of promoting the development and the interchange of ideas and results in the fields devoted to the information technologies applied to the health sciences.

Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions. Telemedicine is sometimes used as a synonym, or is used in a more limited sense to describe remote clinical services, such as diagnosis and monitoring. When rural settings, lack of transport, a lack of mobility, conditions due to outbreaks, epidemics or pandemics, decreased funding, or a lack of staff restrict access to care, telehealth may bridge the gap as well as provide distance-learning; meetings, supervision, and presentations between practitioners; online information and health data management and healthcare system integration. Telehealth could include two clinicians discussing a case over video conference; a robotic surgery occurring through remote access; physical therapy done via digital monitoring instruments, live feed and application combinations; tests being forwarded between facilities for interpretation by a higher specialist; home monitoring through continuous sending of patient health data; client to practitioner online conference; or even videophone interpretation during a consult.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Key components of eHealth include electronic health records (EHRs), telemedicine, health information exchange, mobile health applications, wearable devices, and online health information. These technologies enable healthcare providers, patients, and other stakeholders to access, manage, and exchange health information more effectively, leading to improved communication, decision-making, and overall healthcare outcomes.

Telenursing refers to the use of information technology in the provision of nursing services whenever physical distance exists between patient and nurse, or between any number of nurses. As a field, it is part of telemedicine, and has many points of contacts with other medical and non-medical applications, such as telediagnosis, teleconsultation, and telemonitoring. The field, however, is still being developed as the information on telenursing isn't comprehensive enough.

Telerehabilitation (or e-rehabilitation is the delivery of rehabilitation services over telecommunication networks and the internet. Telerehabilitation allows patients to interact with providers remotely and can be used both to assess patients and to deliver therapy. Fields of medicine that utilize telerehabilitation include: physical therapy, occupational therapy, speech-language pathology, audiology, and psychology. Therapy sessions can be individual or community-based. Types of therapy available include motor training exercises, speech therapy, virtual reality, robotic therapy, goal setting, and group exercise.

Telepsychiatry or telemental health refers to the use of telecommunications technology to deliver psychiatric care remotely for people with mental health conditions. It is a branch of telemedicine.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
Home automation for the elderly and disabled focuses on making it possible for older adults and people with disabilities to remain at home, safe and comfortable. Home automation is becoming a viable option for older adults and people with disabilities who would prefer to stay in the comfort of their homes rather than move to a healthcare facility. This field uses much of the same technology and equipment as home automation for security, entertainment, and energy conservation but tailors it towards old people and people with disabilities.
Connected health is a socio-technical model for healthcare management and delivery by using technology to provide healthcare services remotely. Connected health, also known as technology enabled care (TEC) aims to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care. It uses readily available consumer technologies to deliver patient care outside of the hospital or doctor's office. Connected health encompasses programs in telehealth, remote care and disease and lifestyle management, often leverages existing technologies such as connected devices using cellular networks and is associated with efforts to improve chronic care. However, there is an increasing blur between software capabilities and healthcare needs whereby technologists are now providing the solutions to support consumer wellness and provide the connectivity between patient data, information and decisions. This calls for new techniques to guide Connected Health solutions such as "design thinking" to support software developers in clearly identifying healthcare requirements, and extend and enrich traditional software requirements gathering techniques.

A doctor's visit, also known as a physician office visit or a consultation, or a ward round in an inpatient care context, is a meeting between a patient with a physician to get health advice or treatment plan for a symptom or condition, most often at a professional health facility such as a doctor's office, clinic or hospital. According to a survey in the United States, a physician typically sees between 50 and 100 patients per week, but it may vary with medical specialty, but differs only little by community size such as metropolitan versus rural areas.

Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.
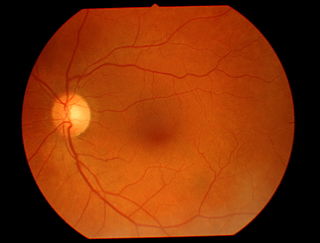
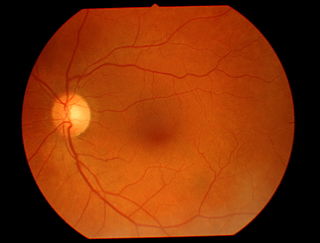
Teleophthalmology is a branch of telemedicine that delivers eye care through digital medical equipment and telecommunications technology. Today, applications of teleophthalmology encompass access to eye specialists for patients in remote areas, ophthalmic disease screening, diagnosis and monitoring; as well as distant learning.

Medical image sharing is the electronic exchange of medical images between hospitals, physicians and patients. Rather than using traditional media, such as a CD or DVD, and either shipping it out or having patients carry it with them, technology now allows for the sharing of these images using the cloud. The primary format for images is DICOM. Typically, non-image data such as reports may be attached in standard formats like PDF during the sending process. Additionally, there are standards in the industry, such as IHE Cross Enterprise Document Sharing for Imaging (XDS-I), for managing the sharing of documents between healthcare enterprises. A typical architecture involved in setup is a locally installed server, which sits behind the firewall, allowing secure transmissions with outside facilities. In 2009, the Radiological Society of North America launched the "Image Share" project, with the goal of giving patients control of their imaging histories by allowing them to manage these records as they would online banking or shopping.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.
American Well Corporation, doing business as Amwell, is a telemedicine company based in Boston, Massachusetts, that connects patients with doctors over secure video. Amwell sells its platform as a subscription service to healthcare providers to put their medical professionals online and its proprietary software development kits, APIs, and system integrations enable clients to embed telehealth into existing workflows utilized by providers and patients.
Credentialing is the process of establishing the qualifications of licensed medical professionals and assessing their background and legitimacy.
Teladoc Health, Inc. is a multinational telemedicine and virtual healthcare company headquartered in the United States. Primary services include telehealth, medical opinions, AI and analytics, telehealth devices and licensable platform services. In particular, Teladoc Health uses telephone and videoconferencing software as well as mobile apps to provide on-demand remote medical care.
Jacqueline Nwando Olayiwola is an American family physician, public health professional, author, professor, and women's empowerment leader. She is the Senior Vice President and Chief Health Equity Officer of Humana and a chair and Professor in the Department of Family Medicine at Ohio State University Wexner Medical Center. Prior to her appointment at OSU, she served as the inaugural Chief Clinical Transformation Officer for RubiconMD, an eConsult platform that improves primary care access to specialty care for underserved patients. Olayiwola is dedicated to serving marginalized patient populations and addressing the social determinants through community and technology-based infrastructures of healthcare reform. She has published articles on the use of eConsults and telehealth to provide underserved patients with primary care treatments so that they have a low cost and efficient means of reaching specialized care. Olayiwola has founded numerous non-profits and healthcare start-ups such as GIRLTALK Inc, Inspire Health Solutions LLC, and the Minority Women Professionals are MVPs Program. She has been recognized at the national and international level for her work and efforts to educate, advocate and provide healthcare to those in need. She was named Woman of the Year by the American Telemedicine Association in 2019, and received the Public Health Innovator Award from Harvard School of Public Health in 2019, as well as being named one of America's Top Family Doctors from 2007 to 2008 by the Consumers Research Council of America.

Before the COVID-19 pandemic, telehealth adoption was gradually increasing. Some patients preferred in-person consultations and expressed concerns about privacy during video calls. However, with the outbreak of COVID-19 in early 2020, healthcare professionals reduced in-person visits to minimize exposure. As a result, telehealth usage surged dramatically, experiencing a 5,000% increase from February to March 2020. Telehealth has since remained widely utilized in healthcare services.