Antimicrobial resistance (AMR) occurs when microbes evolve mechanisms that protect them from the effects of antimicrobials. All classes of microbes can evolve resistance. Fungi evolve antifungal resistance. Viruses evolve antiviral resistance. Protozoa evolve antiprotozoal resistance, and bacteria evolve antibiotic resistance. Bacteria that are considered extensively drug resistant (XDR) or totally drug-resistant (TDR) are sometimes referred to as a superbug. Although antimicrobial resistance is a naturally-occurring process, it is often the result of improper usage of the drugs and management of the infections.

Campylobacteriosis is an infection by the Campylobacter bacterium, most commonly C. jejuni. It is among the most common bacterial infections of humans, often a foodborne illness. It produces an inflammatory, sometimes bloody, diarrhea or dysentery syndrome, mostly including cramps, fever and pain.
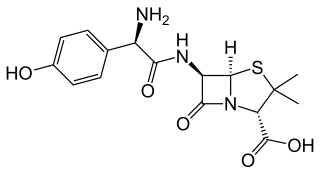
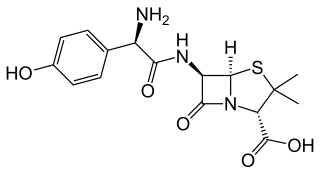
Amoxicillin/clavulanic acid, also known as co-amoxiclav or amox-clav, sold under the brand name Augmentin, among others, is an antibiotic medication used for the treatment of a number of bacterial infections. It is a combination consisting of amoxicillin, a β-lactam antibiotic, and potassium clavulanate, a β-lactamase inhibitor. It is specifically used for otitis media, streptococcal pharyngitis, pneumonia, cellulitis, urinary tract infections, and animal bites. It is taken by mouth or by injection into a vein.

There are different systems of feeding cattle in animal husbandry. For pastured animals, grass is usually the forage that composes the majority of their diet. Cattle reared in feedlots are fed hay supplemented with grain, soy and other ingredients to increase the energy density of the feed. The debate is whether cattle should be raised on fodder primarily composed of grass or a concentrate. The issue is complicated by the political interests and confusion between labels such as "free range", "organic", or "natural". Cattle raised on a primarily foraged diet are termed grass-fed or pasture-raised; for example meat or milk may be called grass-fed beef or pasture-raised dairy. The term "pasture-raised" can lead to confusion with the term "free range", which does not describe exactly what the animals eat.
Multiple drug resistance (MDR), multidrug resistance or multiresistance is antimicrobial resistance shown by a species of microorganism to at least one antimicrobial drug in three or more antimicrobial categories. Antimicrobial categories are classifications of antimicrobial agents based on their mode of action and specific to target organisms. The MDR types most threatening to public health are MDR bacteria that resist multiple antibiotics; other types include MDR viruses, parasites.
Carbadox is a veterinary drug that combats infection in swine, particularly swine dysentery.
Natural growth promoters (NGPs) are feed additives for farm animals.

Enrofloxacin (ENR) is a fluoroquinolone antibiotic sold by the Bayer Corporation under the trade name Baytril. It is sold by in a generic form by Bimeda Inc. under the name EnroMed 100. Enrofloxacin is currently approved by the FDA for the treatment of individual pets and domestic animals in the United States. In September 2005, the FDA withdrew approval of Baytril for use in water to treat flocks of poultry, as this practice was noted to promote the evolution of fluoroquinolone-resistant strains of the bacterium Campylobacter, a human pathogen.
Enterococcus faecium is a Gram-positive, gamma-hemolytic or non-hemolytic bacterium in the genus Enterococcus. It can be commensal in the gastrointestinal tract of humans and animals, but it may also be pathogenic, causing diseases such as neonatal meningitis or endocarditis.

Intensive animal farming or industrial livestock production, also known by its opponents as factory farming and macro-farms, is a type of intensive agriculture, specifically an approach to animal husbandry designed to maximize production, while minimizing costs. To achieve this, agribusinesses keep livestock such as cattle, poultry, and fish at high stocking densities, at large scale, and using modern machinery, biotechnology, and global trade. The main products of this industry are meat, milk and eggs for human consumption. There are issues regarding whether intensive animal farming is sustainable in the social long-run given its costs in resources. Analysts also raise issues about its ethics.

The environmental impacts of animal agriculture vary because of the wide variety of agricultural practices employed around the world. Despite this, all agricultural practices have been found to have a variety of effects on the environment. Animal agriculture, in particular meat production can cause pollution, greenhouse gas emissions, biodiversity loss, disease, and significant consumption of land, food, and water. Meat is obtained through a variety of methods, including organic farming, free range farming, intensive livestock production and subsistence agriculture. The livestock sector also includes wool, and egg and dairy production, the livestock used for tillage, and fish farming.

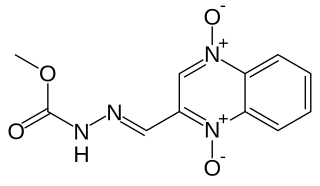
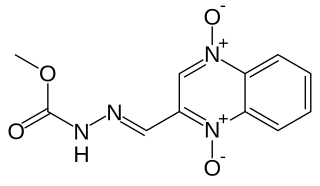
Flumequine is a synthetic fluoroquinolone antibiotic used to treat bacterial infections. It is a first-generation fluoroquinolone antibacterial that has been removed from clinical use and is no longer being marketed. The marketing authorization of flumequine has been suspended throughout the EU. It kills bacteria by interfering with the enzymes that cause DNA to unwind and duplicate. Flumequine was used in veterinarian medicine for the treatment of enteric infections, as well as to treat cattle, swine, chickens, and fish, but only in a limited number of countries. It was occasionally used in France to treat urinary tract infections under the trade name Apurone. However this was a limited indication because only minimal serum levels were achieved.

Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria can develop resistance to multiple antibiotics and cause life-threatening infections.

A quinolone antibiotic is a member of a large group of broad-spectrum bacteriocidals that share a bicyclic core structure related to the substance 4-quinolone. They are used in human and veterinary medicine to treat bacterial infections, as well as in animal husbandry, specifically poultry production.

Antibiotics are commonly used in commercial swine production in the United States and around the world. They are used for disease treatment, disease prevention and control, and growth promotion. When used for growth promoting purposes, antibiotics are given at low concentrations for long periods of time. Low concentration of antibiotics, also referred to as subtherapeutic (STA), are given as feed and water additives which improve daily weight gain and feed efficiency through alterations in digestion and disease suppression. Additionally, the use of STA in swine results in healthier animals and reduces the “microbial load” on meat resulting in an assumed decrease in potential Foodborne illness risk. While the benefits of subtherapeutic antibiotic administration are well-documented, there is much concern and debate regarding the development of bacterial antibiotic resistance associated with their use.
Antimicrobials destroy bacteria, viruses, fungi, algae, and other microbes. The cells of bacteria (prokaryotes), such as salmonella, differ from those of higher-level organisms (eukaryotes), such as fish. Antibiotics are chemicals designed to either kill or inhibit the growth of pathogenic bacteria while exploiting the differences between prokaryotes and eukaryotes in order to make them relatively harmless in higher-level organisms. Antibiotics are constructed to act in one of three ways: by disrupting cell membranes of bacteria, by impeding DNA or protein synthesis, or by hampering the activity of certain enzymes unique to bacteria.

Antibiotic use in livestock is the use of antibiotics for any purpose in the husbandry of livestock, which includes treatment when ill (therapeutic), treatment of a group of animals when at least one is diagnosed with clinical infection (metaphylaxis), and preventative treatment (prophylaxis). Antibiotics are an important tool to treat animal as well as human disease, safeguard animal health and welfare, and support food safety. However, used irresponsibly, this may lead to antibiotic resistance which may impact human, animal and environmental health.
Antimicrobial resistance (AMR) directly kills about 1,600 people each year in Australia. This is a currently serious threat to both humans and animals in the country. Antimicrobial resistance occurs when a microorganism evolves and gains the ability to become more resistant or completely resistant to the medicine that was previously used to treat it. Drug-resistant bacteria are increasingly difficult to treat, requiring replacement or higher-dose drugs that may be more expensive or more toxic. Resistance can develop through one of the three mechanisms: natural resistant ability in some types of microorganisms, a mutation in genes or receiving the resistance from another species. Antibodies appear naturally due to random mutations, or more often after gradual accumulation over time, and because of abuse of antibiotics. Multidrug-resistance, or MDR, are the microorganisms that are resistant to many types of antimicrobials. "Superbugs" is the term also used for multidrug-resistant microbes, or totally drug-resistant (TDR).
The Veterinary Drugs Directorate is the Canadian body responsible for putting all "veterinary products, such antimicrobials, growth promotion drugs and feed additives, through a rigorous approval process before they are licensed and sold for use" in Canada. It is part of the Health Products and Food Branch of Health Canada, and exists by virtue of the Food and Drugs Act. Its goal is "to protect human and animal health and the safety of Canada's food supply."
Antibiotics in poultry farming in America is the controversial prophylactic use of antibiotics in the country's poultry farming industry. This does not represent the position in other countries.