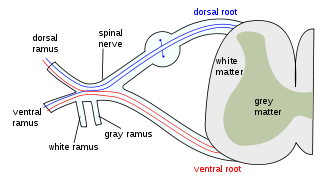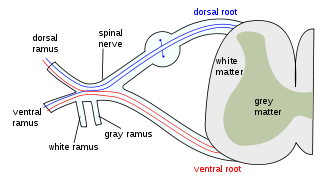
A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the corresponding cervical, thoracic, lumbar, sacral and coccygeal regions of the spine. There are eight pairs of cervical nerves, twelve pairs of thoracic nerves, five pairs of lumbar nerves, five pairs of sacral nerves, and one pair of coccygeal nerves. The spinal nerves are part of the peripheral nervous system.

A discectomy is the surgical removal of abnormal disc material that presses on a nerve root or the spinal cord. The procedure involves removing a portion of an intervertebral disc, which causes pain, weakness or numbness by stressing the spinal cord or radiating nerves. The traditional open discectomy, or Love's technique, was published by Ross and Love in 1971. Advances have produced visualization improvements to traditional discectomy procedures, or endoscopic discectomy. In conjunction with the traditional discectomy or microdiscectomy, a laminotomy is often involved to permit access to the intervertebral disc. Laminotomy means a significant amount of typically normal bone is removed from the vertebra, allowing the surgeon to better see and access the area of disc herniation.

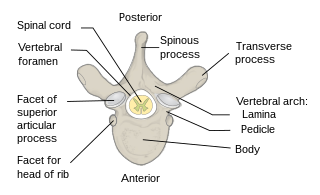
Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
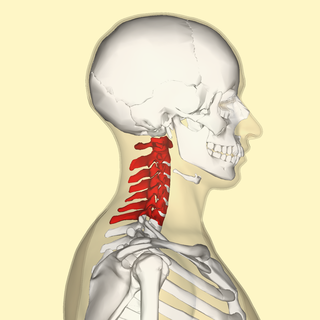
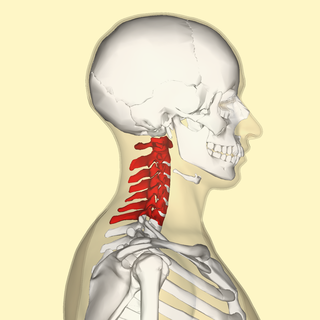
In tetrapods, cervical vertebrae are the vertebrae of the neck, immediately below the skull. Truncal vertebrae lie caudal of cervical vertebrae. In sauropsid species, the cervical vertebrae bear cervical ribs. In lizards and saurischian dinosaurs, the cervical ribs are large; in birds, they are small and completely fused to the vertebrae. The vertebral transverse processes of mammals are homologous to the cervical ribs of other amniotes. Most mammals have seven cervical vertebrae, with the only three known exceptions being the manatee with six, the two-toed sloth with five or six, and the three-toed sloth with nine.

A cervical fracture, commonly called a broken neck, is a fracture of any of the seven cervical vertebrae in the neck. Examples of common causes in humans are traffic collisions and diving into shallow water. Abnormal movement of neck bones or pieces of bone can cause a spinal cord injury, resulting in loss of sensation, paralysis, or usually death soon thereafter, primarily via compromising neurological supply to the respiratory muscles as well as innervation to the heart.

Degenerative disc disease (DDD) is a medical condition typically brought on by the normal aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.
Bone morphogenetic proteins (BMPs) are a group of growth factors also known as cytokines and as metabologens. Originally discovered by their ability to induce the formation of bone and cartilage, BMPs are now considered to constitute a group of pivotal morphogenetic signals, orchestrating tissue architecture throughout the body. The important functioning of BMP signals in physiology is emphasized by the multitude of roles for dysregulated BMP signalling in pathological processes. Cancerous disease often involves misregulation of the BMP signalling system. Absence of BMP signalling is, for instance, an important factor in the progression of colon cancer, and conversely, overactivation of BMP signalling following reflux-induced esophagitis provokes Barrett's esophagus and is thus instrumental in the development of esophageal adenocarcinoma.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a neurosurgical or orthopedic surgical technique that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.

A spinal disc herniation is an injury to the cushioning and connective tissue between vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including posture.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

Cervical spinal stenosis is a bone disease involving the narrowing of the spinal canal at the level of the neck. It is frequently due to chronic degeneration, but may also be congenital. Treatment is frequently surgical.

Laminoplasty is an orthopaedic/neurosurgical surgical procedure for treating spinal stenosis by relieving pressure on the spinal cord. The main purpose of this procedure is to provide relief to patients who may have symptoms of numbness, pain, or weakness in arm movement. The procedure involves cutting the lamina on both sides of the affected vertebrae and then "swinging" the freed flap of bone open thus relieving the pressure on the spinal cord. The spinous process may be removed to allow the lamina bone flap to be swung open. The bone flap is then propped open using small wedges or pieces of bone such that the enlarged spinal canal will remain in place.

A spinal fracture, also called a vertebral fracture or a broken back, is a fracture affecting the vertebrae of the spinal column. Most types of spinal fracture confer a significant risk of spinal cord injury. After the immediate trauma, there is a risk of spinal cord injury if the fracture is unstable, that is, likely to change alignment without internal or external fixation.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.
Minimally invasive spine surgery, also known as MISS, has no specific meaning or definition. It implies a lack of severe surgical invasion. The older style of open-spine surgery for a relatively small disc problem used to require a 5-6 inch incision and a month in the hospital. MISS techniques utilize more modern technology, advanced imaging techniques and special medical equipment to reduce tissue trauma, bleeding, radiation exposure, infection risk, and decreased hospital stays by minimizing the size of the incision. Modern endoscopic procedures can be done through a 2 to 5 mm skin opening. By contrast, procedures done with a microscope require skin openings of approximately one inch, or more.
The ventral slot technique is a procedure that allows the surgeon to reach and decompress the spinal cord and associated nerve roots from a ventral route in veterinary medicine. There are also alternative ways to open the spinal canal from dorsal by performing a hemilaminectomy, but this often gives only limited access. Even when the main pathological changes evolve from the midline, it is necessary to choose a ventral approach.
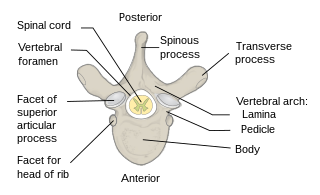
The spinal column, a defining synapomorphy shared by nearly all vertebrates, is a moderately flexible series of vertebrae, each constituting a characteristic irregular bone whose complex structure is composed primarily of bone, and secondarily of hyaline cartilage. They show variation in the proportion contributed by these two tissue types; such variations correlate on one hand with the cerebral/caudal rank, and on the other with phylogenetic differences among the vertebrate taxa.

Cervicocranial syndrome or is a neurological illness. It is a combination of symptoms that are caused by an abnormality in the neck. The bones of the neck that are affected are cervical vertebrae. This syndrome can be identified by confirming cervical bone shifts, collapsed cervical bones or misalignment of the cervical bone leading to improper functioning of cervical spinal nerves. Cervicocranial syndrome is either congenital or acquired. Some examples of diseases that could result in cervicocranial syndrome are Chiari disease, Klippel-Feil malformation osteoarthritis, and trauma. Treatment options include neck braces, pain medication and surgery. The quality of life for individuals suffering from CCJ syndrome can improve through surgery.
The Philadelphia Surgery Center is a medical facility in Narberth, Pennsylvania, that specializes in small-scale endoscopic spine surgery for the treatment of spinal stenosis and herniated or fragmented spinal discs.

Thomas Schuler, M.D., F.A.C.S is an American spinal surgeon, researcher and educator in the treatment of neck and low back conditions. He was an early adopter of stem cell therapy, biologics, robotics, laser and hybrid surgery and augmented reality for spinal surgery. Schuler specializes in cervical and lumbar disc replacement procedures, minimally invasive spine surgery and robotic spine surgery. He performed the first hybrid multi-level cervical artificial disc replacement with spinal fusion in the country. He founded a practice that has performed some of the first robotic and augmented reality spinal surgeries in the world. In 2002 he created and currently serves as President of the National Spine Health Foundation, a national non-profit focused on education, research and patient advocacy of neck and back health.