Related Research Articles

Mammography is the process of using low-energy X-rays to examine the human breast for diagnosis and screening. The goal of mammography is the early detection of breast cancer, typically through detection of characteristic masses or microcalcifications.

Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined for the presence of prostate cancer. It is typically performed when the result from a PSA blood test is high. It may also be considered advisable after a digital rectal exam (DRE) finds possible abnormality. PSA screening is controversial as PSA may become elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH), by infection, or by manipulation of the prostate during surgery or catheterization. Additionally many prostate cancers detected by screening develop so slowly that they would not cause problems during a man's lifetime, making the complications due to treatment unnecessary.
The American College of Radiology (ACR), founded in 1923, is a professional medical society representing nearly 40,000 diagnostic radiologists, radiation oncologists, interventional radiologists, nuclear medicine physicians and medical physicists.
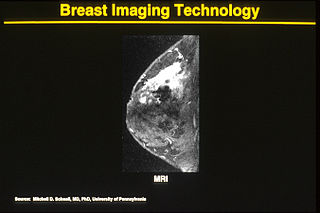
One alternative to mammography, breast MRI or contrast-enhanced magnetic resonance imaging (MRI), has shown substantial progress in the detection of breast cancer.

The Mammography Quality Standards Act (MQSA) was enacted by the United States Congress to regulate the quality of care in mammography. The act was officially effective in 1994, and was extended in 2004 to continue through 2007. The U.S. Food and Drug Administration (FDA) began inspections of mammography facilities to ensure compliance in 1995. In 1997, more comprehensive regulation was added to become effective in 1999.
A breast cyst is a cyst, a fluid-filled sac, within the breast. One breast can have one or more cysts. They are often described as round or oval lumps with distinct edges. In texture, a breast cyst usually feels like a soft grape or a water-filled balloon, but sometimes a breast cyst feels firm.

Thyroid nodules are nodules which commonly arise within an otherwise normal thyroid gland. They may be hyperplastic or tumorous, but only a small percentage of thyroid tumors are malignant. Small, asymptomatic nodules are common, and often go unnoticed. Nodules that grow larger or produce symptoms may eventually need medical care. A goitre may have one nodule – uninodular, multiple nodules – multinodular, or be diffuse.

Breast cancer screening is the medical screening of asymptomatic, apparently healthy women for breast cancer in an attempt to achieve an earlier diagnosis. The assumption is that early detection will improve outcomes. A number of screening tests have been employed, including clinical and self breast exams, mammography, genetic screening, ultrasound, and magnetic resonance imaging.

Molecular breast imaging (MBI), also known as scintimammography, is a type of breast imaging test that is used to detect cancer cells in breast tissue of individuals who have had abnormal mammograms, especially for those who have dense breast tissue, post-operative scar tissue or breast implants.
Daniel B. Kopans, MD, FACR is a radiologist specializing in mammography and other forms of breast imaging.
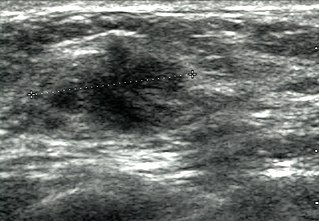
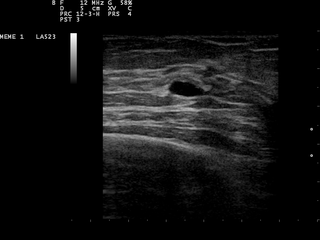
Breast ultrasound is a medical imaging technique that uses medical ultrasonography to perform imaging of the breast. It can be performed for either diagnostic or screening purposes and can be used with or without a mammogram. In particular, breast ultrasound may be useful for younger women who have denser fibrous breast tissue that may make mammograms more challenging to interpret.

A breast biopsy is usually done after a suspicious lesion is discovered on either mammography or ultrasound to get tissue for pathological diagnosis. Several methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality. The different types of breast biopsies include fine-needle aspiration (FNA), vacuum-assisted biopsy, core needle biopsy, and surgical excision biopsy. Breast biopsies can be done utilizing ultrasound, MRI or a stereotactic biopsy imaging guidance. Vacuum assisted biopsies are typically done using stereotactic techniques when the suspicious lesion can only be seen on mammography. On average, 5–10 biopsies of a suspicious breast lesion will lead to the diagnosis of one case of breast cancer. Needle biopsies have largely replaced open surgical biopsies in the initial assessment of imaging as well as palpable abnormalities in the breast.

The triple test score is a diagnostic tool for examining potentially cancerous breasts. Diagnostic accuracy of the triple test score is nearly 100%. Scoring includes using the procedures of physical examination, mammography and needle biopsy. If the results of a triple test score are greater than five, an excisional biopsy is indicated.
Dynamic angiothermography (DATG) is a technique for the diagnosis of breast cancer. This technique, though springing from the previous conception of thermography, is based on a completely different principle. DATG records the temperature variations linked to the vascular changes in the breast due to angiogenesis. The presence, change, and growth of tumors and lesions in breast tissue change the vascular network in the breast. Consequently, through measuring the vascular structure over time, DATG effectively monitors the change in breast tissue due to tumors and lesions. It is currently used in combination with other techniques for diagnosis of breast cancer. This diagnostic method is a low-cost one compared with other techniques.
Automated whole-breast ultrasound (AWBU) is a medical imaging technique used in radiology to obtain volumetric ultrasound data of the entire breast.
The Canadian National Breast Screening Study, sometimes abbreviated as CNBSS or NBSS, was a randomized trial conducted with the aim of evaluating whether mammography reduced breast cancer incidence or mortality among women who underwent screening. The trial was initiated in 1980, and was conducted in fifteen screening centers in six different Canadian provinces. It was the first study designed to determine whether mammography was effective among women between the ages of 40 and 49.
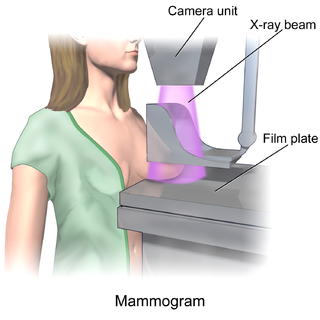
In medicine, breast imaging is a sub-speciality of diagnostic radiology that involves imaging of the breasts for screening or diagnostic purposes. There are various methods of breast imaging using a variety of technologies as described in detail below. Traditional screening and diagnostic mammography uses x-ray technology and has been the mainstay of breast imaging for many decades. Breast tomosynthesis is a relatively new digital x-ray mammography technique that produces multiple image slices of the breast similar to, but distinct from, computed tomography (CT). Xeromammography and galactography are somewhat outdated technologies that also use x-ray technology and are now used infrequently in the detection of breast cancer. Breast ultrasound is another technology employed in diagnosis and screening that can help differentiate between fluid filled and solid lesions, an important factor to determine if a lesion may be cancerous. Breast MRI is a technology typically reserved for high-risk patients and patients recently diagnosed with breast cancer. Lastly, scintimammography is used in a subgroup of patients who have abnormal mammograms or whose screening is not reliable on the basis of using traditional mammography or ultrasound.

The Liver Imaging Reporting and Data System is a quality assurance tool created and trademarked by the American College of Radiology in 2011 to standardize the reporting and data collection of CT and MR imaging patients at risk for hepatocellular carcinoma (HCC), or primary cancer of the liver cells. It provides a standardized framework for classification of liver lesions by a radiologist, and only applies in patients with chronic liver disease, the main risk factor for liver cancer. The hierarchical classification, from LR1 to LR5, is based on specific imaging features of the lesion in question, and corresponds to the degree of suspicion for malignancy. For example, a lesion with features corresponding to the highest category, LR5, is "definitely" HCC. Importantly, the increasing acceptance of the LI-RADS system of reporting by referring clinicians has reduced the need for tissue biopsy confirmation of cancer in patients with chronic liver disease.
HB 2102, also known as "Henda's Law", is a breast density (BD) notification law approved in 2011 by the FDA that mammography patients be provided educational materials on dense breast tissue can hide abnormalities, including breast cancer, from traditional screening. Henda's Law aims to promote patient–doctor discussion as well as reduce the rate of false negatives, as mammography may not detect abnormalities in dense breasts.
Dense breast tissue, also known as dense breasts, is a condition of the breasts where a higher proportion of the breasts are made up of glandular tissue and fibrous tissue than fatty tissue. Around 40–50% of women have dense breast tissue and one of the main medical components of the condition is that mammograms are unable to differentiate tumorous tissue from the surrounding dense tissue. This increases the risk of late diagnosis of breast cancer in women with dense breast tissue. Additionally, women with such tissue have a higher likelihood of developing breast cancer in general, though the reasons for this are poorly understood.
References
- ↑ Mehrjardi MZ (2015). "Bi-RADS® for: mammography and ultrasound (2013 updated version) (PDF Download Available)". ResearchGate. doi:10.13140/rg.2.2.24908.82562/1.
- ↑ American College of Radiology (ACR) Breast Imaging Reporting and Data System Atlas (BI-RADS Atlas). Reston, Va: © American College of Radiology; 2003
- ↑ ACR Practice Guideline for the Performance of Ultrasound-Guided Percutaneous Breast Interventional Procedures Res. 29; American College of Radiology; 2009
- ↑ Sanders MA, Roland L, Sahoo S (2010). "Clinical Implications of Subcategorizing BI-RADS 4 Breast Lesions associated with Microcalcification: A Radiology–Pathology Correlation Study". The Breast Journal. 16 (1): 28–31. doi: 10.1111/j.1524-4741.2009.00863.x . PMID 19929890. S2CID 9585100.
- ↑ D'Orsi CJ, Sickles EA, Mendelson EB, Morris EA, et al. (2013). ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology.
- ↑ Nassif H, Woods R, Burnside E, Ayvaci M, Shavlik J, Page D (2009). "Information Extraction for Clinical Data Mining: A Mammography Case Study" (PDF). 2009 IEEE International Conference on Data Mining Workshops. Miami. pp. 37–42. doi:10.1109/icdmw.2009.63. ISBN 978-1-4244-5384-9. PMC 3676897 . PMID 23765123.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Nassif H, Cunha F, Moreira IC, Cruz-Correia R, Sousa E, Page D, Burnside E, Dutra I (2012). "Extracting BI-RADS features from Portuguese clinical texts". 2012 IEEE International Conference on Bioinformatics and Biomedicine. pp. 539–542. doi:10.1109/bibm.2012.6392613. ISBN 978-1-4673-2560-8. PMC 3688645 . PMID 23797461.
- ↑ Sippo DA, Warden GI, Andriole KP, Lacson R, Ikuta I, Birdwell RL, Khorasani R (2013). "Automated Extraction of BI-RADS Final Assessment Categories from Radiology Reports with Natural Language Processing". Journal of Digital Imaging. 26 (5): 989–994. doi:10.1007/s10278-013-9616-5. PMC 3782591 . PMID 23868515.
- ↑ Percha B, Nassif H, Lipson J, Burnside E, Rubin D (2012). "Automatic classification of mammography reports by BI-RADS breast tissue composition class". Journal of the American Medical Informatics Association. 19 (5): 913–916. doi:10.1136/amiajnl-2011-000607. PMC 3422822 . PMID 22291166.
- ↑ Banerjee I, Bozkurt S, Alkim E, Sagreiya H, Kurian AW, Rubin DL (2019-04-01). "Automatic inference of BI-RADS final assessment categories from narrative mammography report findings". Journal of Biomedical Informatics. 92: 103137. doi:10.1016/j.jbi.2019.103137. PMC 6462247 . PMID 30807833.