Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

A hepatocyte is a cell of the main parenchymal tissue of the liver. Hepatocytes make up 80% of the liver's mass. These cells are involved in:

Steatosis, also called fatty change, is abnormal retention of fat (lipids) within a cell or organ. Steatosis most often affects the liver – the primary organ of lipid metabolism – where the condition is commonly referred to as fatty liver disease. Steatosis can also occur in other organs, including the kidneys, heart, and muscle. When the term is not further specified, it is assumed to refer to the liver.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.

Fatty liver disease (FLD), also known as hepatic steatosis and steatotic liver disease (SLD), is a condition where excess fat builds up in the liver. Often there are no or few symptoms. Occasionally there may be tiredness or pain in the upper right side of the abdomen. Complications may include cirrhosis, liver cancer, and esophageal varices.

Kupffer cells, also known as stellate macrophages and Kupffer–Browicz cells, are specialized cells localized in the liver within the lumen of the liver sinusoids and are adhesive to their endothelial cells which make up the blood vessel walls. Kupffer cells comprise the largest population of tissue-resident macrophages in the body. Gut bacteria, bacterial endotoxins, and microbial debris transported to the liver from the gastrointestinal tract via the portal vein will first come in contact with Kupffer cells, the first immune cells in the liver. It is because of this that any change to Kupffer cell functions can be connected to various liver diseases such as alcoholic liver disease, viral hepatitis, intrahepatic cholestasis, steatohepatitis, activation or rejection of the liver during liver transplantation and liver fibrosis. They form part of the mononuclear phagocyte system.

Cell death is the event of a biological cell ceasing to carry out its functions. This may be the result of the natural process of old cells dying and being replaced by new ones, as in programmed cell death, or may result from factors such as diseases, localized injury, or the death of the organism of which the cells are part. Apoptosis or Type I cell-death, and autophagy or Type II cell-death are both forms of programmed cell death, while necrosis is a non-physiological process that occurs as a result of infection or injury.

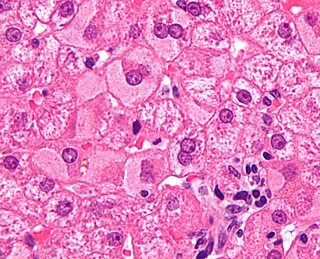
In histopathology, a Mallory body, Mallory–Denk body (MDB), or Mallory's hyaline is an inclusion found in the cytoplasm of liver cells. Mallory bodies are damaged intermediate filaments within the liver cells.
Cell damage is a variety of changes of stress that a cell suffers due to external as well as internal environmental changes. Amongst other causes, this can be due to physical, chemical, infectious, biological, nutritional or immunological factors. Cell damage can be reversible or irreversible. Depending on the extent of injury, the cellular response may be adaptive and where possible, homeostasis is restored. Cell death occurs when the severity of the injury exceeds the cell's ability to repair itself. Cell death is relative to both the length of exposure to a harmful stimulus and the severity of the damage caused. Cell death may occur by necrosis or apoptosis.

Cytopathic effect(abbreviated CPE) refers to structural changes in host cells that are caused by viral invasion. The infecting virus causes lysis of the host cell or when the cell dies without lysis due to an inability to replicate. If a virus causes these morphological changes in the host cell, it is said to be cytopathogenic. Common examples of CPE include rounding of the infected cell, fusion with adjacent cells to form syncytia, and the appearance of nuclear or cytoplasmic inclusion bodies.

The fatty-acid-binding proteins (FABPs) are a family of transport proteins for fatty acids and other lipophilic substances such as eicosanoids and retinoids. These proteins are thought to facilitate the transfer of fatty acids between extra- and intracellular membranes. Some family members are also believed to transport lipophilic molecules from outer cell membrane to certain intracellular receptors such as PPAR. The FABPs are intracellular carriers that “solubilize” the endocannabinoid anandamide (AEA), transporting AEA to the breakdown by FAAH, and compounds that bind to FABPs block AEA breakdown, raising its level. The cannabinoids are also discovered to bind human FABPs that function as intracellular carriers, as THC and CBD inhibit the cellular uptake and catabolism of AEA by targeting FABPs. Competition for FABPs may in part or wholly explain the increased circulating levels of endocannabinoids reported after consumption of cannabinoids. Levels of fatty-acid-binding protein have been shown to decline with ageing in the mouse brain, possibly contributing to age-associated decline in synaptic activity.
In cell biology and pathophysiology, cellular adaptation refers to changes made by a cell in response to adverse or varying environmental changes. The adaptation may be physiologic (normal) or pathologic (abnormal).

In cellular neuroscience, chromatolysis is the dissolution of the Nissl bodies in the cell body of a neuron. It is an induced response of the cell usually triggered by axotomy, ischemia, toxicity to the cell, cell exhaustion, virus infections, and hibernation in lower vertebrates. Neuronal recovery through regeneration can occur after chromatolysis, but most often it is a precursor of apoptosis. The event of chromatolysis is also characterized by a prominent migration of the nucleus towards the periphery of the cell and an increase in the size of the nucleolus, nucleus, and cell body. The term "chromatolysis" was initially used in the 1940s to describe the observed form of cell death characterized by the gradual disintegration of nuclear components; a process which is now called apoptosis. Chromatolysis is still used as a term to distinguish the particular apoptotic process in the neuronal cells, where Nissl substance disintegrates.
Transneuronal degeneration is the death of neurons resulting from the disruption of input from or output to other nearby neurons. It is an active excitotoxic process when a neuron is overstimulated by a neurotransmitter causing the dysfunction of that neuron which drives neighboring neurons into metabolic deficit, resulting in rapid, widespread loss of neurons. This can be either anterograde or retrograde, indicating the direction of the degeneration relative to the original site of damage. There are varying causes for transneuronal degeneration such as brain lesions, disconnection syndromes, respiratory chain deficient neuron interaction, and lobectomies. Although there are different causes, transneuronal degeneration generally results in the same effects to varying degrees. Transneuronal degeneration is thought to be linked to a number of diseases, most notably Huntington's disease and Alzheimer's disease, and researchers recently have been performing experiments with monkeys and rats, monitoring lesions in different parts of the body to study more closely how exactly the process works.
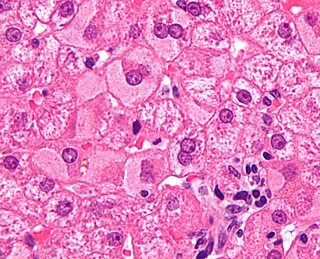
In liver pathology, a ground glass hepatocyte, abbreviated GGH, is a liver parenchymal cell with a flat hazy and uniformly dull appearing cytoplasm on light microscopy. The cytoplasm's granular homogeneous eosinophilic staining is caused by the presence of HBsAg.

In histopathology, feathery degeneration, formally feathery degeneration of hepatocytes, is a form of liver parenchymal cell death associated with cholestasis.
Liver cytology is the branch of cytology that studies the liver cells and its functions. The liver is a vital organ, in charge of almost all the body’s metabolism. Main liver cells are hepatocytes, Kupffer cells, and hepatic stellate cells; each one with a specific function.
Hepatokines are proteins produced by liver cells (hepatocytes) that are secreted into the circulation and function as hormones across the organism. Research is mostly focused on hepatokines that play a role in the regulation of metabolic diseases such as diabetes and fatty liver and include: Adropin, ANGPTL4, Fetuin-A, Fetuin-B, FGF-21, Hepassocin, LECT2, RBP4,Selenoprotein P, Sex hormone-binding globulin.