Cardiac arrest, also known as sudden cardiac arrest, is when the heart suddenly and unexpectedly stops beating. As a result blood will not be pumped around the body in normal circulation, consciousness will be rapidly lost, and breathing will be abnormal or absent. Without immediate intervention such as cardiopulmonary resuscitation (CPR), and possibly defibrillation, death will occur within minutes.

An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.
Human body weight is a person's mass or weight.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).
In physiology and medicine, the body surface area (BSA) is the measured or calculated surface area of a human body. For many clinical purposes, BSA is a better indicator of metabolic mass than body weight because it is less affected by abnormal adipose mass. Nevertheless, there have been several important critiques of the use of BSA in determining the dosage of medications with a narrow therapeutic index, such as chemotherapy.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.

An inhaler is a medical device used for delivering medicines into the lungs through the work of a person's breathing. This allows medicines to be delivered to and absorbed in the lungs, which provides the ability for targeted medical treatment to this specific region of the body, as well as a reduction in the side effects of oral medications. There are a wide variety of inhalers, and they are commonly used to treat numerous medical conditions with asthma and chronic obstructive pulmonary disease (COPD) being among the most notable.
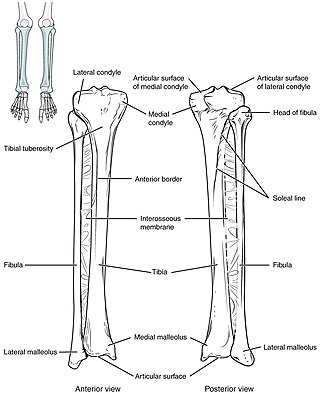
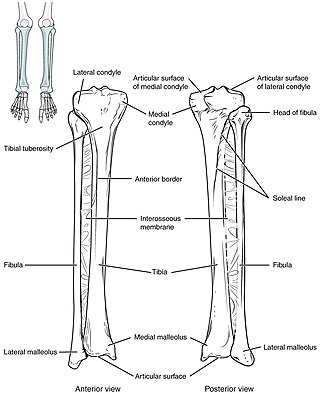
Intraosseous infusion (IO) is the process of injecting medications, fluids, or blood products directly into the marrow of a bone; this provides a non-collapsible entry point into the systemic venous system. The intraosseous infusion technique is used to provide fluids and medication when intravenous access is not available or not feasible. Intraosseous infusions allow for the administered medications and fluids to go directly into the vascular system. The IO route of fluid and medication administration is an alternative to the preferred intravascular route when the latter cannot be established promptly in emergent situations. Intraosseous infusions are used when people have compromised intravenous access and need immediate delivery of life-saving fluids and medications.

In the United States, the paramedic is a allied health professional whose primary focus is to provide advanced emergency medical care for patients who access Emergency Medical Services (EMS). This individual possesses the complex knowledge and skills necessary to provide patient care and transportation. Paramedics function as part of a comprehensive EMS response under physician medical direction. Paramedics often serve in a prehospital role, responding to Public safety answering point (9-1-1) calls in an ambulance. The paramedic serves as the initial entry point into the health care system. A standard requirement for state licensure involves successful completion of a nationally accredited Paramedic program at the certificate or associate degree level.
In medicine, intravascular volume status refers to the volume of blood in a patient's circulatory system, and is essentially the blood plasma component of the overall volume status of the body, which otherwise includes both intracellular fluid and extracellular fluid. Still, the intravascular component is usually of primary interest, and volume status is sometimes used synonymously with intravascular volume status.
Clark's rule is a medical term referring to a mathematical formula used to calculate the proper dosage of medicine for children aged 2–17 based on the weight of the patient and the appropriate adult dose. The formula was named after Cecil Belfield Clarke (1894–1970), a Barbadian physician who practiced throughout the UK, the West Indies and Ghana.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.

Trauma in children, also known as pediatric trauma, refers to a traumatic injury that happens to an infant, child or adolescent. Because of anatomical and physiological differences between children and adults the care and management of this population differs.
Paediatric radiology is a subspecialty of radiology involving the imaging of fetuses, infants, children, adolescents and young adults. Many paediatric radiologists practice at children's hospitals.
The Pediatric Assessment Triangle or PAT is a tool used in emergency medicine to form a general impression of a pediatric patient. In emergency medicine, a general impression is formed the first time the medical professional views the patient, usually within seconds. The PAT is a method of quickly determining the acuity of the child, identifying the type of pathophysiology, e.g., respiratory distress, respiratory failure, or shock and establishing urgency for treatment. The PAT also drives initial resuscitation and stabilization efforts based on the assessment findings.

Rearrest is a phenomenon that involves the resumption of a lethal cardiac dysrhythmia after successful return of spontaneous circulation (ROSC) has been achieved during the course of resuscitation. Survival to hospital discharge rates are as low as 7% for cardiac arrest in general and although treatable, rearrest may worsen these survival chances. Rearrest commonly occurs in the out-of-hospital setting under the treatment of health care providers.
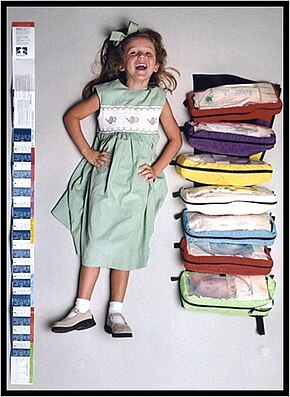
James Broselow is an American emergency physician, an assistant professor, an inventor and an entrepreneur. He and fellow emergency physician Robert Luten, M.D., are best known in the medical community for inventing the Broselow Tape in 1985, which was the first tool developed relating a pediatric patient's height to their weight in order to “determine the size of equipment, supplies, and dosages of medication to use…” during emergencies. The Broselow Tape is featured in many medical textbooks and reference manuals as the standard for length based weight measures.
Renal angina is a clinical methodology to risk stratify patients for the development of persistent and severe acute kidney injury (AKI). The composite of risk factors and early signs of injury for AKI, renal angina is used as a clinical adjunct to help optimize the use of novel AKI biomarker testing. The term angina from Latin and from the Greek ankhone ("strangling") are utilized in the context of AKI to denote the development of injury and the choking off of kidney function. Unlike angina pectoris, commonly caused due to ischemia of the heart muscle secondary to coronary artery occlusion or vasospasm, renal angina carries no obvious physical symptomatology. Renal angina was derived as a conceptual framework to identify evolving AKI. Like acute coronary syndrome which precedes or is a sign of a heart attack, renal angina is used as a herald sign for a kidney attack. Detection of renal angina is performed by calculating the renal angina index.

The Wallace rule of nines is a tool used in pre-hospital and emergency medicine to estimate the total body surface area (BSA) affected by a burn. In addition to determining burn severity, the measurement of burn surface area is important for estimating patients' fluid requirements and determining hospital admission criteria.
The JumpSTART pediatric triage MCI triage tool is a variation of the simple triage and rapid treatment (START) triage system. Both systems are used to sort patients into categories at mass casualty incidents (MCIs). However, JumpSTART was designed specifically for triaging children in disaster settings. Though JumpSTART was developed for use in children from infancy to age 8, where age is not immediately obvious, it is used in any patient who appears to be a child.