Marburg virus disease is a viral hemorrhagic fever in human and non-human primates caused by either of the two Marburgviruses: Marburg virus (MARV) and Ravn virus (RAVV). Its clinical symptoms are very similar to those of Ebola virus disease (EVD).

The 1978 smallpox outbreak in the United Kingdom resulted in the death of Janet Parker, a British medical photographer, who became the last recorded person to die from smallpox. Her illness and death, which was connected to the deaths of two other people, led to the Shooter Inquiry, an official investigation by government-appointed experts triggering radical changes in how dangerous pathogens were studied in the UK and named after the panel's leader.

The Prince of Wales Hospital is a 440-bed major public teaching hospital located in Sydney's eastern suburb of Randwick, providing a full range of hospital services to the people of New South Wales, Australia. The hospital has strong ties to the adjacent University of New South Wales. The Prince of Wales Hospital shares the Randwick Hospitals' Campus site with the Sydney Children's Hospital and the Royal Hospital for Women, as well as the Prince of Wales Private Hospital.
Catherine-de-Barnes is a small village within the Metropolitan Borough of Solihull in the English county of West Midlands. It is situated about 2.25 miles east of Solihull town centre, in the civil parish of Hampton in Arden, and 2 miles west of Hampton village. Population as taken in the 2011 census can be found under Bickenhill.

Ali Maow Maalin was a Somali hospital cook and health worker from Merca who is the last person known to have been infected with naturally occurring Variola minor smallpox. He was diagnosed with the disease in October 1977 and made a full recovery. Although he had many contacts, none of them developed the disease, and an aggressive containment campaign was successful in preventing an outbreak. Smallpox was declared to have been eradicated globally by the World Health Organization (WHO) two years later. Maalin was subsequently involved in the successful poliomyelitis eradication campaign in Somalia, and he died of malaria while carrying out polio vaccinations after the re-emergence of the poliovirus in 2013.
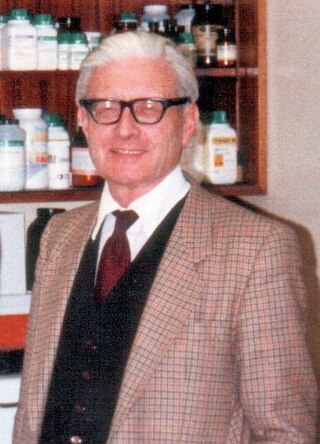
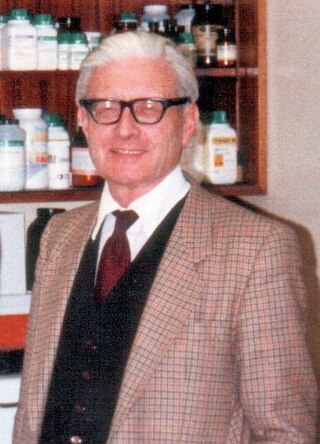
Thomas Henry Flewett, MD, FRCPath, FRCP was a founder member of the Royal College of Pathologists and was elected a Fellow of the Royal College of Physicians of London in 1978. He was chairman of the World Health Organization (WHO) Steering Committee on Viral Diarrhoeal Diseases, 1990–3, and a member until 1996. His laboratory in Birmingham was a World Health Organization Reference and Research Centre for Rotavirus Infections from 1980 until his retirement in 1987. He was an external examiner, visiting lecturer, and scientific journal editor. He was a member of the board of the Public Health Laboratory Service from 1977 to 1983 and was chairman of the Public Health Laboratory Service's Committee on Electron Microscopy from 1977 to 1987.
Historically, puerperal fever was a devastating disease. It affected women within the first three days after childbirth and progressed rapidly, causing acute symptoms of severe abdominal pain, fever and debility.

In hospitals and other medical facilities, an isolation ward is a separate ward used to isolate patients with infectious diseases. Several wards for individual patients are usually placed together in an isolation unit.

Lodge Moor Hospital is a former isolation hospital on Redmires Road in the Lodge Moor area of the City of Sheffield, England. The hospital which opened in 1888 and closed in 1994 initially treated Smallpox but soon broadened its treatment to other infectious diseases and in its latter years expanded to provide more general nursing, notably spinal injuries and chest medicine. At the time of closure, the hospital was operated by the Central Sheffield University Hospitals NHS Trust.

Ruchill Hospital was a fever hospital in the Ruchill area of Glasgow, Scotland. The hospital was closed in 1998 and was sold to Scottish Enterprise in July 1999. It was managed by NHS Greater Glasgow.
The 1947 New York City smallpox outbreak occurred in March 1947 and was declared ended on April 24, 1947. The outbreak marked the largest mass vaccination effort ever conducted for smallpox in America. Within three weeks of the discovery of the outbreak, the U.S. Public Health Service, in conjunction with New York City health officials, had procured the smallpox vaccine and inoculated over 6,350,000 adults and children. Of that number, 5,000,000 had been vaccinated within the first two weeks. The rapid response was credited with limiting the outbreak to 12 people, 10 of whom recovered, while 2 died.

King's Cross Hospital, often shortened to King's Cross is a hospital in Dundee, Scotland. It is managed by NHS Tayside.

Heartlands Hospital is an acute general hospital in Bordesley Green, Birmingham, England. It is managed by University Hospitals Birmingham NHS Foundation Trust.
Witton Isolation Hospital was a facility for the treatment and quarantine of smallpox victims and their contacts in Birmingham, England, from 1894 to 1966.
Monsall Hospital was a hospital in North Manchester, England.

An outbreak of smallpox in Bradford in 1962 first came to attention on 11 January 1962, when a cook from the children's hospital in Bradford, West Riding of Yorkshire, England, presented with an unexplained fever and was found to have changes in her blood similar to another sick person at the nearby St Luke's Hospital, both samples appearing compatible with smallpox. The index case was later discovered to be a nine-year old girl who arrived in the UK on 16 December 1961 from Karachi, Pakistan, where there was an ongoing epidemic of smallpox.
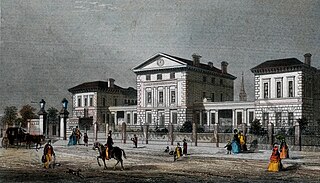
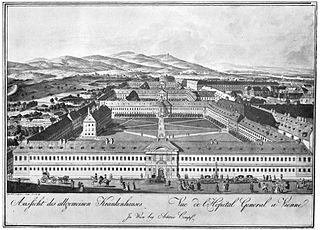
A fever hospital or isolation hospital is a hospital for infectious diseases such as Scarlet fever, Tuberculosis, Lassa fever and Smallpox. Their purpose is to treat affected people while isolating them from the general population. Early examples included the Liverpool Fever Hospital (1801) and the London Fever Hospital (1802). Other examples occurred elsewhere in the British Isles and India.
Alasdair Macintosh Geddes was a British medical doctor who was Professor of Infection at the University of Birmingham Medical School. In 1978, as the World Health Organization (WHO) was shortly to announce that the world's last case of smallpox had occurred a year earlier in Somalia, Geddes diagnosed a British woman with the disease in Birmingham, England. She was found to be the index case of the outbreak and became the world's last reported fatality due to the disease, five years after he had gained experience on the frontline of the WHO's smallpox eradication programme in Bangladesh in 1973.

The Edinburgh City Hospital was a hospital in Colinton, Edinburgh, opened in 1903 for the treatment of infectious diseases. As the pattern of infectious disease changed, the need for in-patients facilities to treat them diminished. While still remaining the regional centre for infectious disease, in the latter half of the 20th century the hospital facilities diversified with specialist units established for respiratory disease, ear, nose and throat surgery, maxillo-facial surgery, care of the elderly and latterly HIV/AIDS. The hospital closed in 1999 and was redeveloped as residential housing, known as Greenbank Village.
In the 2020 dengue outbreak in Singapore, a record-breaking number of dengue fever cases was reported in Singapore. This was part of the wider 2019–2020 dengue fever epidemic which also affected several neighbouring countries in Southeast Asia.