The lungs are the main organs of the respiratory system in most terrestrial animals, including all tetrapod vertebrates and a small number of amphibious fish, pulmonate gastropods, and some arachnids. Their function is to conduct gas exchange by extracting oxygen from the air into the bloodstream via diffusion, and to release carbon dioxide from the bloodstream out into the atmosphere, a process also known as respiration. This article primarily concerns with the lungs of tetrapods, which are paired and located on either side of the heart, occupying most of the volume of the thoracic cavity, and are homologous to the swim bladders in ray-finned fish.

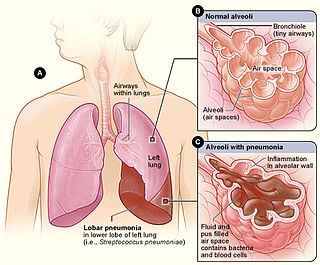
A pulmonary alveolus, also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the lungs where pulmonary gas exchange takes place. Oxygen is exchanged for carbon dioxide at the blood–air barrier between the alveolar air and the pulmonary capillary. Alveoli make up the functional tissue of the mammalian lungs known as the lung parenchyma, which takes up 90 percent of the total lung volume.

The respiratory tract is the subdivision of the respiratory system involved with the process of conducting air to the alveoli for the purposes of gas exchange in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

The bronchioles are the smaller branches of the bronchial airways in the lower respiratory tract. They include the terminal bronchioles, and finally the respiratory bronchioles that mark the start of the respiratory zone delivering air to the gas exchanging units of the alveoli. The bronchioles no longer contain the cartilage that is found in the bronchi, or glands in their submucosa.

Pulmonary surfactant is a surface-active complex of phospholipids and proteins formed by type II alveolar cells. The proteins and lipids that make up the surfactant have both hydrophilic and hydrophobic regions. By adsorbing to the air-water interface of alveoli, with hydrophilic head groups in the water and the hydrophobic tails facing towards the air, the main lipid component of surfactant, dipalmitoylphosphatidylcholine (DPPC), reduces surface tension.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
The pores of Kohn are discrete holes in walls of adjacent alveoli. Cuboidal type II alveolar cells, which produce surfactant, usually form part of aperture.
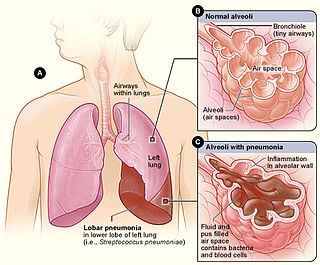
Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung.

Alveolar lung diseases, are a group of diseases that mainly affect the alveoli of the lungs.
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation. Pulmonary function test demonstrates a decrease in the forced vital capacity.

Mucociliary clearance (MCC), mucociliary transport, or the mucociliary escalator describes the self-clearing mechanism of the airways in the respiratory system. It is one of the two protective processes for the lungs in removing inhaled particles including pathogens before they can reach the delicate tissue of the lungs. The other clearance mechanism is provided by the cough reflex. Mucociliary clearance has a major role in pulmonary hygiene.

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.

Pulmonary interstitial emphysema (PIE) is a collection of air outside of the normal air space of the pulmonary alveoli, found instead inside the connective tissue of the peribronchovascular sheaths, interlobular septa, and visceral pleura. This collection of air develops as a result of alveolar and terminal bronchiolar rupture. Pulmonary interstitial emphysema is more frequent in premature infants who require mechanical ventilation for severe lung disease. Infants with pulmonary interstitial emphysema are typically recommended for admission to a neonatal intensive care unit.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the permanent enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.
Bronchoscopic lung volume reduction(BLVR) is a procedure to reduce the volume of air within the lungs. BLVR was initially developed in the early 2000s as a minimally invasive treatment for severe COPD that is primarily caused by emphysema. BLVR evolved from earlier surgical approaches first developed in the 1950s to reduce lung volume by removing damaged portions of the lungs via pneumonectomy or wedge resection. Procedures include the use of valves, coils, or thermal vapour ablation.

Ventilation–perfusion coupling is the relationship between ventilation and perfusion processes, which take place in the respiratory system and the cardiovascular system. Ventilation is the movement of gas during breathing, and perfusion is the process of pulmonary blood circulation, which delivers oxygen to body tissues. Anatomically, the lung structure, alveolar organization, and alveolar capillaries contribute to the physiological mechanism of ventilation and perfusion. Ventilation–perfusion coupling maintains a constant ventilation/perfusion ratio near 0.8 on average, while the regional variation exists within the lungs due to gravity. When the ratio gets above or below 0.8, it is considered abnormal ventilation-perfusion coupling, also known as a ventilation–perfusion mismatch. Lung diseases, cardiac shunts, and smoking can cause a ventilation-perfusion mismatch that results in significant symptoms and diseases, which can be treated through treatments like bronchodilators and oxygen therapy.
Whole lung lavage (WLL), also called lung washing, is a medical procedure in which the patient's lungs are washed with saline by filling and draining repeatedly. It is used to treat pulmonary alveolar proteinosis, in which excess lung surfactant proteins prevent the patient from breathing. Some sources consider it a variation of bronchoalveolar lavage.