Apraxia is a motor disorder caused by damage to the brain, which causes difficulty with motor planning to perform tasks or movements. The nature of the damage determines the disorder's severity, and the absence of sensory loss or paralysis helps to explain the level of difficulty. Children may be born with apraxia; its cause is unknown, and symptoms are usually noticed in the early stages of development. Apraxia occurring later in life, known as acquired apraxia, is typically caused by traumatic brain injury, stroke, dementia, Alzheimer's disease, brain tumor, or other neurodegenerative disorders. The multiple types of apraxia are categorized by the specific ability and/or body part affected.
Agraphia is an acquired neurological disorder causing a loss in the ability to communicate through writing, either due to some form of motor dysfunction or an inability to spell. The loss of writing ability may present with other language or neurological disorders; disorders appearing commonly with agraphia are alexia, aphasia, dysarthria, agnosia, acalculia and apraxia. The study of individuals with agraphia may provide more information about the pathways involved in writing, both language related and motoric. Agraphia cannot be directly treated, but individuals can learn techniques to help regain and rehabilitate some of their previous writing abilities. These techniques differ depending on the type of agraphia.
Alien hand syndrome (AHS) or Dr. Strangelove syndrome is a category of conditions in which a person experiences their limbs acting seemingly on their own, without conscious control over the actions. There are a variety of clinical conditions that fall under this category, which most commonly affects the left hand. There are many similar terms for the various forms of the condition, but they are often used inappropriately. The affected person may sometimes reach for objects and manipulate them without wanting to do so, even to the point of having to use the controllable hand to restrain the alien hand. Under normal circumstances however, given that intent and action can be assumed to be deeply mutually entangled, the occurrence of alien hand syndrome can be usefully conceptualized as a phenomenon reflecting a functional "disentanglement" between thought and action.

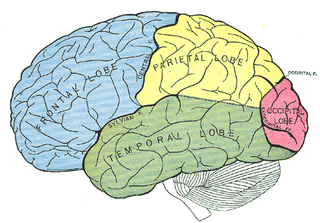
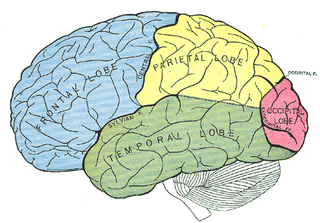
The parietal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The parietal lobe is positioned above the temporal lobe and behind the frontal lobe and central sulcus.
Anosognosia is a condition in which a person with a disability is cognitively unaware of having it due to an underlying physical condition. Anosognosia results from physiological damage to brain structures, typically to the parietal lobe or a diffuse lesion on the fronto-temporal-parietal area in the right hemisphere, and is thus a neuropsychiatric disorder. A deficit of self-awareness, the term was first coined by the neurologist Joseph Babinski in 1914, in order to describe the unawareness of hemiplegia.

Hemispatial neglect is a neuropsychological condition in which, after damage to one hemisphere of the brain, a deficit in attention and awareness towards the side of space opposite brain damage is observed. It is defined by the inability of a person to process and perceive stimuli towards the contralesional side of the body or environment. Hemispatial neglect is very commonly contralateral to the damaged hemisphere, but instances of ipsilesional neglect have been reported.
Bálint's syndrome is an uncommon and incompletely understood triad of severe neuropsychological impairments: inability to perceive the visual field as a whole (simultanagnosia), difficulty in fixating the eyes, and inability to move the hand to a specific object by using vision. It was named in 1909 for the Austro-Hungarian neurologist and psychiatrist Rezső Bálint who first identified it.

Visual memory describes the relationship between perceptual processing and the encoding, storage and retrieval of the resulting neural representations. Visual memory occurs over a broad time range spanning from eye movements to years in order to visually navigate to a previously visited location. Visual memory is a form of memory which preserves some characteristics of our senses pertaining to visual experience. We are able to place in memory visual information which resembles objects, places, animals or people in a mental image. The experience of visual memory is also referred to as the mind's eye through which we can retrieve from our memory a mental image of original objects, places, animals or people. Visual memory is one of several cognitive systems, which are all interconnected parts that combine to form the human memory. Types of palinopsia, the persistence or recurrence of a visual image after the stimulus has been removed, is a dysfunction of visual memory.
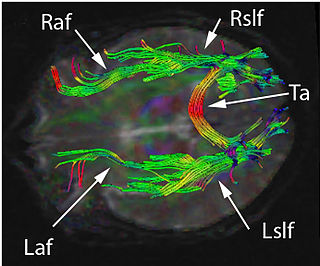
The two-streams hypothesis is a model of the neural processing of vision as well as hearing. The hypothesis, given its initial characterisation in a paper by David Milner and Melvyn A. Goodale in 1992, argues that humans possess two distinct visual systems. Recently there seems to be evidence of two distinct auditory systems as well. As visual information exits the occipital lobe, and as sound leaves the phonological network, it follows two main pathways, or "streams". The ventral stream leads to the temporal lobe, which is involved with object and visual identification and recognition. The dorsal stream leads to the parietal lobe, which is involved with processing the object's spatial location relative to the viewer and with speech repetition.
Ideomotor Apraxia, often IMA, is a neurological disorder characterized by the inability to correctly imitate hand gestures and voluntarily mime tool use, e.g. pretend to brush one's hair. The ability to spontaneously use tools, such as brushing one's hair in the morning without being instructed to do so, may remain intact, but is often lost. The general concept of apraxia and the classification of ideomotor apraxia were developed in Germany in the late 19th and early 20th centuries by the work of Hugo Liepmann, Adolph Kussmaul, Arnold Pick, Paul Flechsig, Hermann Munk, Carl Nothnagel, Theodor Meynert, and linguist Heymann Steinthal, among others. Ideomotor apraxia was classified as "ideo-kinetic apraxia" by Liepmann due to the apparent dissociation of the idea of the action with its execution. The classifications of the various subtypes are not well defined at present, however, owing to issues of diagnosis and pathophysiology. Ideomotor apraxia is hypothesized to result from a disruption of the system that relates stored tool use and gesture information with the state of the body to produce the proper motor output. This system is thought to be related to the areas of the brain most often seen to be damaged when ideomotor apraxia is present: the left parietal lobe and the premotor cortex. Little can be done at present to reverse the motor deficit seen in ideomotor apraxia, although the extent of dysfunction it induces is not entirely clear.

Integrative agnosia is a sub-disease of agnosia, meaning the lack of integrating perceptual wholes within knowledge. Integrative agnosia can be assessed by several experimental tests such as the Efron shape test, which determines the specificity of the disease being Integrative. This disease is often caused by brain trauma, producing medial ventral lesions to the extrastriate cortex. Affecting this region of the brain produces learning impairments: the inability to integrate parts such as spatial distances or producing visual images from short or long-term memory.
Ideational apraxia (IA) is a neurological disorder which explains the loss of ability to conceptualize, plan, and execute the complex sequences of motor actions involved in the use of tools or otherwise interacting with objects in everyday life. Ideational apraxia is a condition in which an individual is unable to plan movements related to interaction with objects, because they have lost the perception of the object's purpose. Characteristics of this disorder include a disturbance in the concept of the sequential organization of voluntary actions. The patient appears to have lost the knowledge or thought of what an object represents. This disorder was first seen 100 years ago by Doctor Arnold Pick, who described a patient who appeared to have lost their ability to use objects. The patient would make errors such as combing their hair with the wrong side of the comb or placing a pistol in his mouth. From that point on, several other researchers and doctors have stumbled upon this unique disorder. IA has been described under several names such as, agnosia of utilization, conceptual apraxia or loss of knowledge about the use of tools, or Semantic amnesia of tool usage. The term apraxia was first created by Steinthal in 1871 and was then applied by Gogol, Kusmaul, Star, and Pick to patients who failed to pantomime the use of tools. It was not until the 1900s, when Liepmann refined the definition, that it specifically described disorders that involved motor planning, rather than disturbances in the patient’s visual perception, language, or symbolism.
The neuroanatomy of memory encompasses a wide variety of anatomical structures in the brain.

Gerstmann syndrome is a neuropsychological disorder that is characterized by a constellation of symptoms that suggests the presence of a lesion usually near the junction of the temporal and parietal lobes at or near the angular gyrus. Gerstmann syndrome is typically associated with damage to the inferior parietal lobule of the dominant hemisphere. It is classically considered a left-hemisphere disorder, although right-hemisphere damage has also been associated with components of the syndrome.

Allochiria is a neurological disorder in which the patient responds to stimuli presented to one side of their body as if the stimuli had been presented at the opposite side. It is associated with spatial transpositions, usually symmetrical, of stimuli from one side of the body to the opposite one. Thus a touch to the left side of the body will be reported as a touch to the right side, which is also known as somatosensory allochiria. If the auditory or visual senses are affected, sounds will be reported as being heard on the opposite side to that on which they occur and objects presented visually will be reported as having been presented on the opposite side. Often patients may express allochiria in their drawing while copying an image. Allochiria often co-occurs with unilateral neglect and, like hemispatial neglect, the disorder arises commonly from damage to the right parietal lobe.
Amorphosynthesis, also called a hemi-sensory deficit, is a neuropsychological condition in which a patient experiences unilateral inattention to sensory input. This phenomenon is frequently associated with damage to the right cerebral hemisphere resulting in severe sensory deficits that are observed on the contralesional (left) side of the body. A right-sided deficit is less commonly observed and the effects are reported to be temporary and minor. Evidence suggests that the right cerebral hemisphere has a dominant role in attention and awareness to somatic sensations through ipsilateral and contralateral stimulation. In contrast, the left cerebral hemisphere is activated only by contralateral stimuli. Thus, the left and right cerebral hemispheres exhibit redundant processing to the right-side of the body and a lesion to the left cerebral hemisphere can be compensated by the ipsiversive processes of the right cerebral hemisphere. For this reason, right-sided amorphosynthesis is less often observed and is generally associated with bilateral lesions.
Topographical disorientation is the inability to orient oneself in one's surroundings, sometimes as a result of focal brain damage. This disability may result from the inability to make use of selective spatial information or to orient by means of specific cognitive strategies such as the ability to form a mental representation of the environment, also known as a cognitive map. It may be part of a syndrome known as visuospatial dysgnosia.
Visuospatial dysgnosia is a loss of the sense of "whereness" in the relation of oneself to one's environment and in the relation of objects to each other. Visuospatial dysgnosia is often linked with topographical disorientation.
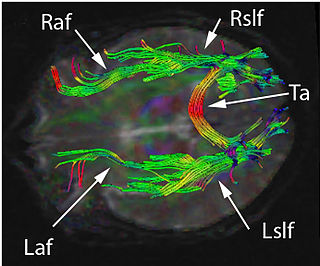
Disconnection syndrome is a general term for a collection of neurological symptoms caused – via lesions to associational or commissural nerve fibres – by damage to the white matter axons of communication pathways in the cerebrum, independent of any lesions to the cortex. The behavioral effects of such disconnections are relatively predictable in adults. Disconnection syndromes usually reflect circumstances where regions A and B still have their functional specializations except in domains that depend on the interconnections between the two regions.

Masud Husain FMedSci is a clinical neurologist and neuroscientist working in the UK. He is Professor of Neurology & Cognitive Neuroscience at the Nuffield Department of Clinical Neurosciences and Departmental of Experimental Psychology, University of Oxford, a Professorial Fellow at New College, Oxford, and Editor-in-Chief of the journal Brain. He was born in East Pakistan.