Related Research Articles

Lambert–Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by muscle weakness of the limbs. It is also known as myasthenic syndrome, Eaton–Lambert syndrome, and when related to cancer, carcinomatous myopathy.
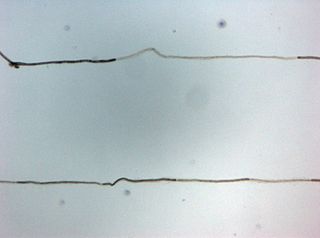
Neuromyotonia (NMT) is a form of peripheral nerve hyperexcitability that causes spontaneous muscular activity resulting from repetitive motor unit action potentials of peripheral origin. NMT along with Morvan's syndrome are the most severe types in the Peripheral Nerve Hyperexciteability spectrum. Example of two more common and less severe syndromes in the spectrum are cramp fasciculation syndrome and benign fasciculation syndrome. NMT can have both hereditary and acquired (non-inherited) forms. The prevalence of NMT is unknown.
Morvan's syndrome is a rare, life-threatening autoimmune disease named after the nineteenth century French physician Augustin Marie Morvan. "La chorée fibrillaire" was first coined by Morvan in 1890 when describing patients with multiple, irregular contractions of the long muscles, cramping, weakness, pruritus, hyperhidrosis, insomnia and delirium. It normally presents with a slow insidious onset over months to years. Approximately 90% of cases spontaneously go into remission, while the other 10% of cases lead to death.

Benign fasciculation syndrome (BFS) is characterized by fasciculation (twitching) of voluntary muscles in the body. The twitching can occur in any voluntary muscle group but is most common in the eyelids, arms, hands, fingers, legs, and feet. The tongue can also be affected. The twitching may be occasional to continuous. BFS must be distinguished from other conditions that include muscle twitches.
Myotonia is a symptom of a small handful of certain neuromuscular disorders characterized by delayed relaxation of the skeletal muscles after voluntary contraction or electrical stimulation, and the muscle shows an abnormal EMG.

Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

A fasciculation, or muscle twitch, is a spontaneous, involuntary muscle contraction and relaxation, involving fine muscle fibers. They are common, with as many as 70% of people experiencing them. They can be benign, or associated with more serious conditions. When no cause or pathology is identified, they are diagnosed as benign fasciculation syndrome.

Stiff-person syndrome (SPS), also known as stiff-man syndrome, is a rare neurological disorder of unclear cause characterized by progressive muscular rigidity and stiffness. The stiffness primarily affects the truncal muscles and is characterised by spasms, resulting in postural deformities. Chronic pain, impaired mobility, and lumbar hyperlordosis are common symptoms.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Myositis is a rarely-encountered medical condition characterized by inflammation affecting the muscles. The manifestations of this condition may include skin issues, muscle weakness, and the potential involvement of other organs. Additionally, systemic symptoms like weight loss, fatigue, and low-grade fever can manifest in individuals with myositis.

A neuromuscular disease is any disease affecting the peripheral nervous system (PNS), the neuromuscular junctions, or skeletal muscles, all of which are components of the motor unit. Damage to any of these structures can cause muscle atrophy and weakness. Issues with sensation can also occur.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
A paraneoplastic syndrome is a syndrome that is the consequence of a tumor in the body. It is specifically due to the production of chemical signaling molecules by tumor cells or by an immune response against the tumor. Unlike a mass effect, it is not due to the local presence of cancer cells.
Ian Kirkland Hart FRCP was a lecturer and consultant in neurology at the Walton Centre in Liverpool. He ran a clinic for neurological paraneoplastic syndromes, myasthenia gravis, neuromyotonia, Lambert–Eaton myasthenic syndrome and autoimmune encephalitis. He was also the founder member of the Walton Centre Clinical Neuroimmunology Group researching on autoantibody-associated neurological diseases.

Brody myopathy, also called Brody disease, is a rare disorder that affects skeletal muscle function. BD was first characterized in 1969 by Dr. Irwin A. Brody at Duke University Medical Center. Individuals with BD have difficulty relaxing their muscles after exercise. This difficulty in relaxation leads to symptoms including cramps, stiffness, and discomfort in the muscles of the limbs and face. Symptoms are heightened by exercise and commonly progress in severity throughout adulthood.
Multifocal motor neuropathy (MMN) is a progressively worsening condition where muscles in the extremities gradually weaken. The disorder, a pure motor neuropathy syndrome, is sometimes mistaken for amyotrophic lateral sclerosis (ALS) because of the similarity in the clinical picture, especially if muscle fasciculations are present. MMN is thought to be autoimmune. It was first described in the mid-1980s.
Anti-VGKC-complex encephalitis are caused by antibodies against the voltage gated potassium channel-complex (VGKC-complex) and are implicated in several autoimmune conditions including limbic encephalitis, epilepsy and neuromyotonia.

Hirayama disease, also known as monomelic amyotrophy (MMA), is a rare motor neuron disease first described in 1959 in Japan. Its symptoms usually appear about two years after adolescent growth spurt and is significantly more common in males, with an average age of onset between 15 and 25 years. Hirayama disease is reported most frequently in Asia but has a global distribution. It is typically marked by insidious onset of muscle atrophy of an upper limb, which plateaus after two to five years from which it neither improves nor worsens. There is no pain or sensory loss. It is not believed to be hereditary.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.

Autosomal recessive axonal neuropathy with neuromyotonia, also known as Gamstorp-Wohlfart syndrome, is a rare hereditary disorder which is characterized by progressive poly-neuropathy, neuromyotonia, myokymia, pseudo-myotonia, hand-foot contractures, and abnormal neuro-myotonic/myokimic activity visible on needle EMG. According to OMIM, around 52 cases have been reported in medical literature However; new cases have been reported since 2014.
References
- ↑ Jansen, P. H. P.; Dijck, J. A. A. M.; Verbeek, A. L. M.; Durian, F. W.; Joosten, E. M. G. (1991). "Estimation of the frequency of the muscular pain-fasciculation syndrome and the muscular cramp-fasciculation syndrome in the adult population". European Archives of Psychiatry and Clinical Neuroscience. 241 (2): 102–4. doi:10.1007/BF02191150. PMID 1834178. S2CID 30203831.
- ↑ Ropper, Allan H.; Brown, Robert H. (2005). "Disorders of Muscle Characterized by Cramp, Spasm, Pain, and Localized Masses". Adams and Victor's Principles of Neurology (8th ed.). New York: McGraw-Hill. pp. 1277–8. ISBN 978-0-07-141620-7.
- ↑ Lagueny, A (2005). "Cramp-fasciculation syndrome". Revue Neurologique. 161 (12 Pt 1): 1260–6. doi:10.1016/S0035-3787(05)85238-5. PMID 16340924.
- ↑ Hart, Ian K.; Maddison, Paul; Newsom-Davis, John; Vincent, Angela; Mills, Kerry R. (2002). "Phenotypic variants of autoimmune peripheral nerve hyperexcitability". Brain. 125 (8): 1887–95. doi: 10.1093/brain/awf178 . PMID 12135978.
- ↑ Washington University in St. Louis, Neuromuscular: Cramp-Fasciculation Syndromes, http://neuromuscular.wustl.edu/mother/activity.html#crampfas
- ↑ Tahmoush, AJ; Alonso, RJ; Tahmoush, GP; Heiman-Patterson, TD (1991). "Cramp-fasciculation syndrome: a treatable hyperexcitable peripheral nerve disorder". Neurology. 41 (7): 1021–4. doi:10.1212/wnl.41.7.1021. PMID 1648679. S2CID 28873053.
- ↑ TeleEMG website, Amyotrophic Lateral Sclerosis (ALS)/Motor Neuron Disease, Page 2 "EMG & Nerve Conductions | EMG F.A.Q : ALS - Page 2". Archived from the original on 2010-11-29. Retrieved 2010-10-27.
- ↑ de Entrambasaguas, Manuel; Ortega-Albás, Juan-José; Martínez-Lozano, María-Dolores; Díaz, José-Ramón (2006). "Bronchial involvement in the cramp-fasciculation syndrome". European Neurology. 56 (2): 124–6. doi:10.1159/000095703. PMID 16960453. S2CID 45080149.
- 1 2 Tahmoush, A. J.; Alonso, R. J.; Tahmoush, G. P.; Heiman-Patterson, T. D. (1991). "Cramp-fasciculation syndrome: A treatable hyperexcitable peripheral nerve disorder". Neurology. 41 (7): 1021–4. doi:10.1212/wnl.41.7.1021. PMID 1648679. S2CID 28873053.
- ↑ Allan H. Ropper; Robert H. Brown. "Chapter 55. Disorders of Muscle". Adams and Victor's Principles of Neurology (8th ed.). pp. 1277–1278.
- ↑ Hart, I.; Maddison, P.; Newsom-Davis, J.; Vincent, A.; Mills, K. R. (August 2002). "Phenotypic Variants of Autoimmune Peripheral Nerve Hyperexcitability". Brain. 125 (8): 1887–1895. doi: 10.1093/brain/awf178 . PMID 12135978.