Related Research Articles
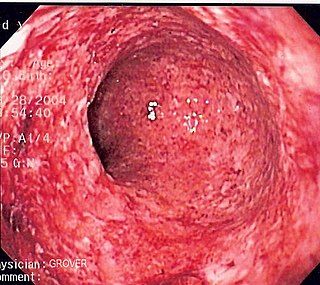
Crohn's disease is a chronic inflammatory bowel disease characterized by recurrent episodes of intestinal inflammation, primarily manifesting as diarrhea and abdominal pain. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the ileum and colon, involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic fatigue, weight loss, and low-grade fevers are common. Organs such as the skin and joints can also be affected. Complications can include bowel obstructions, fistulas, nutrition problems, and an increased risk of intestinal cancers.

Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other type being Crohn's disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer.
Defecation follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus or cloaca. The act has a variety of names ranging from the common, like pooping or crapping, to the technical, e.g. bowel movement, to the obscene (shitting), to the euphemistic, to the juvenile. The topic, usually avoided in polite company, can become the basis for some potty humor.

Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by a group of symptoms that commonly include abdominal pain, abdominal bloating and changes in the consistency of bowel movements. These symptoms may occur over a long time, sometimes for years. IBS can negatively affect quality of life and may result in missed school or work or reduced productivity at work. Disorders such as anxiety, major depression, and chronic fatigue syndrome are common among people with IBS.

Infliximab, a chimeric monoclonal antibody, sold under the brand name Remicade among others, is a medication used to treat a number of autoimmune diseases. This includes Crohn's disease, ulcerative colitis, rheumatoid arthritis, ankylosing spondylitis, psoriasis, psoriatic arthritis, and Behçet's disease. It is given by slow injection into a vein, typically at six- to eight-week intervals.
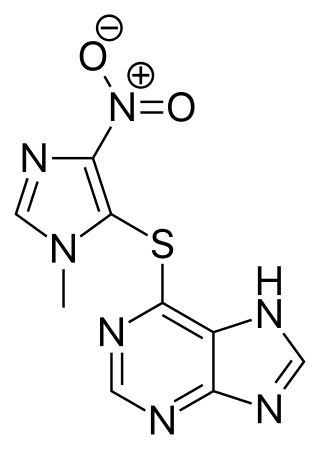
Azathioprine, sold under the brand name Imuran, among others, is an immunosuppressive medication. It is used for the treatment of rheumatoid arthritis, granulomatosis with polyangiitis, Crohn's disease, ulcerative colitis, and systemic lupus erythematosus; and in kidney transplants to prevent rejection. It is listed by the International Agency for Research on Cancer as a group 1 human carcinogen. It is taken by mouth or injected into a vein.
Spondyloarthritis (SpA), also known as spondyloarthropathy, is a collection of clinical syndromes that are connected by genetic predisposition and clinical manifestations. The best-known clinical subtypes are enteropathic arthritis (EA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and reactive arthritis (ReA). Spondyloarthritis typically presents with inflammatory back pain and asymmetrical arthritis, primarily affecting the lower limbs, and enthesitis, inflammation at bone-adhering ligaments, tendons, or joint capsules.

Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas UC primarily affects the colon and the rectum.

A rectovaginal fistula is a medical condition where there is a fistula or abnormal connection between the rectum and the vagina.

Colitis is swelling or inflammation of the large intestine (colon). Colitis may be acute and self-limited or long-term. It broadly fits into the category of digestive diseases.

Diverticular disease is when problems occur due to diverticulosis, a benign condition defined by the formation of pouches (diverticula) from weak spots in the wall of the large intestine. This disease spectrum includes diverticulitis, symptomatic uncomplicated diverticular disease (SUDD), and segmental colitis associated with diverticulosis (SCAD). The most common symptoms across the disease spectrum are abdominal pain and bowel habit changes such as diarrhea or constipation. Otherwise, diverticulitis presents with systemic symptoms such as fever and elevated white blood cell count whereas SUDD and SCAD do not. Treatment ranges from conservative bowel rest to medications such as antibiotics, antispasmodics, acetaminophen, mesalamine, rifaximin, and corticosteroids depending on the specific conditions.
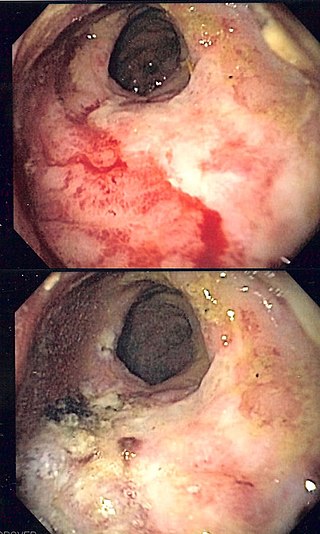
Radiation proctitis or radiation proctopathy is a condition characterized by damage to the rectum after exposure to x-rays or other ionizing radiation as a part of radiation therapy. Radiation proctopathy may occur as acute inflammation called "acute radiation proctitis" or with chronic changes characterized by radiation associated vascular ectasiae (RAVE) and chronic radiation proctopathy. Radiation proctitis most commonly occurs after pelvic radiation treatment for cancers such as cervical cancer, prostate cancer, bladder cancer, and rectal cancer. RAVE and chronic radiation proctopathy involves the lower intestine, primarily the sigmoid colon and the rectum, and was previously called chronic radiation proctitis, pelvic radiation disease and radiation enteropathy.

Collagenous colitis is an inflammatory condition of the colon. Together with the related condition lymphocytic colitis, it is a subtype of microscopic colitis, which is characterized by inflammation that specifically affects the colon, and a clinical presentation that involves watery diarrhea but a lack of rectal bleeding. Microscopic colitis does not usually cause macroscopic changes to the colon that allow a visual diagnosis during colonoscopy, instead causing microscopic changes that can be detected through histopathological examination of colonic biopsies. The nature of these microscopic changes is what differentiates collagenous from lymphocytic colitis, with the characteristic finding in collagenous colitis being depositions of collagen in the connective tissue between the colonic glands. Collagenous colitis, and microscopic colitis as a whole, is sometimes considered to be an inflammatory bowel disease (IBD) along with Crohn's disease and ulcerative colitis. However, little is known about the etiology of microscopic colitis, and so the degree of similarity to the inflammatory bowel diseases is uncertain.
Management of Crohn's disease involves first treating the acute symptoms of the disease, then maintaining remission. Since Crohn's disease is an immune system condition, it cannot be cured by medication or surgery. Treatment initially involves the use of medications to eliminate infections and reduce inflammation. Surgery may be required for complications such as obstructions, fistulae, abscesses, or if the disease does not respond to drugs within a reasonable time. However, surgery cannot cure Crohn's disease. It involves removing the diseased part of the intestine and rejoining the healthy ends, but the disease tends to recur after surgery.

Certolizumab pegol, sold under the brand name Cimzia, is a biopharmaceutical medication for the treatment of Crohn's disease, rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis. It is a fragment of a monoclonal antibody specific to tumor necrosis factor alpha (TNF-α) and is manufactured by UCB.

Biological therapy, the use of medications called biopharmaceuticals or biologics that are tailored to specifically target an immune or genetic mediator of disease, plays a major role in the treatment of inflammatory bowel disease. Even for diseases of unknown cause, molecules that are involved in the disease process have been identified, and can be targeted for biological therapy. Many of these molecules, which are mainly cytokines, are directly involved in the immune system. Biological therapy has found a niche in the management of cancer, autoimmune diseases, and diseases of unknown cause that result in symptoms due to immune related mechanisms.
Vedolizumab, sold under the brand name Entyvio, is a monoclonal antibody medication developed by Takeda Oncology for the treatment of ulcerative colitis and Crohn's disease. It binds to integrin α4β7, blocking the α4β7 integrin results in gut-selective anti-inflammatory activity.

Enteropathic arthropathy commonly referred to as enteropathic arthritis, is a type of arthritis linked to Crohn's disease, ulcerative colitis, and chronic inflammatory bowel diseases.
John Gordon Williams is a British health services researcher and clinical academic gastroenterologist. He led the establishment of the Postgraduate Medical School in Swansea, created and developed the Health Informatics Unit at the Royal College of Physicians, and was the founding president of WAGE, the Welsh Association for Gastroenterology and Endoscopy Williams was appointed a CBE for services to medicine in 2014.
Shomron Ben-Horin is an Israeli physician, a co-founder & Chief Medical Officer of Evinature, and professor of medicine at the Tel-Aviv University.
References
- 1 2 3 Irvine E, Feagan B, Rochon J, Archambault A, Fedorak R, Groll A, Kinnear D, Saibil F, McDonald J (1994). "Quality of life: a valid and reliable measure of therapeutic efficacy in the treatment of inflammatory bowel disease. Canadian Crohn's Relapse Prevention Trial Study Group". Gastroenterology. 106 (2): 287–96. doi:10.1016/0016-5085(94)90585-1. PMID 8299896.
- 1 2 Best WR, Becktel JM, Singleton JW, Kern F Jr (March 1976). "Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study". Gastroenterology. 70 (3): 439–444. doi:10.1016/S0016-5085(76)80163-1. PMID 1248701.
- ↑ Sands B, Anderson F, Bernstein C, Chey W, Feagan B, Fedorak R, Kamm M, Korzenik J, Lashner B, Onken J, Rachmilewitz D, Rutgeerts P, Wild G, Wolf D, Marsters P, Travers S, Blank M, van Deventer S (2004). "Infliximab maintenance therapy for fistulizing Crohn's disease". New England Journal of Medicine. 350 (9): 876–85. doi: 10.1056/NEJMoa030815 . PMID 14985485.
- ↑ Hanauer S, Feagan B, Lichtenstein G, Mayer L, Schreiber S, Colombel J, Rachmilewitz D, Wolf D, Olson A, Bao W, Rutgeerts P (2002). "Maintenance infliximab for Crohn's disease: the ACCENT I randomised trial". Lancet. 359 (9317): 1541–9. doi:10.1016/S0140-6736(02)08512-4. PMID 12047962.
- ↑ Harvey R, Bradshaw J (1980). "A simple index of Crohn's-disease activity". Lancet. 1 (8167): 514. doi:10.1016/S0140-6736(80)92767-1. PMID 6102236.
- ↑ Elliott P, Lennard-Jones J, Hathway N (1980). "Simple index of Crohn's disease activity". Lancet. 1 (8173): 876. doi:10.1016/s0140-6736(80)91372-0. PMID 6103229.
- ↑ Jørgensen L, Fredholm L, Hyltoft Petersen P, Hey H, Munkholm P, Brandslund I (2005). "How accurate are clinical activity indices for scoring of disease activity in inflammatory bowel disease (IBD)?". Clin Chem Lab Med. 43 (4): 403–11. doi:10.1515/CCLM.2005.073. PMID 15899657.
- ↑ Yoshida E (1999). "The Crohn's Disease Activity Index, its derivatives and the Inflammatory Bowel Disease Questionnaire: a review of instruments to assess Crohn's disease". Canadian Journal of Gastroenterology. 13 (1): 65–73. doi: 10.1155/1999/506915 . PMID 10099817.
- ↑ Acciuffi S, Ghosh S, Ferguson A (1996). "Strengths and limitations of the Crohn's disease activity index, revealed by an objective gut lavage test of gastrointestinal protein loss". Alimentary Pharmacology and Therapeutics. 10 (3): 321–6. doi:10.1111/j.0953-0673.1996.00321.x. PMID 8791958.