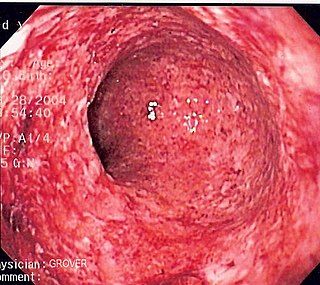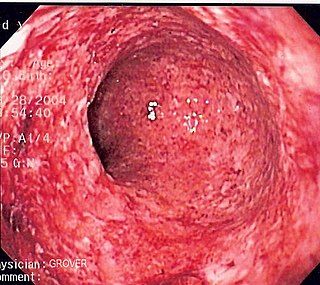
Crohn's disease is a chronic inflammatory bowel disease characterized by recurrent episodes of intestinal inflammation, primarily manifesting as diarrhea and abdominal pain. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the ileum and colon, involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic fatigue, weight loss, and low-grade fevers are common. Organs such as the skin and joints can also be affected. Complications can include bowel obstructions, fistulas, nutrition problems, and an increased risk of intestinal cancers.

An endoscopy is a procedure used in medicine to look inside the body. The endoscopy procedure uses an endoscope to examine the interior of a hollow organ or cavity of the body. Unlike many other medical imaging techniques, endoscopes are inserted directly into the organ.

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".

Fecal occult blood (FOB) refers to blood in the feces that is not visibly apparent. A fecal occult blood test (FOBT) checks for hidden (occult) blood in the stool (feces).

In medicine (gastroenterology), angiodysplasia is a small vascular malformation of the gut. It is a common cause of otherwise unexplained gastrointestinal bleeding and anemia. Lesions are often multiple, and frequently involve the cecum or ascending colon, although they can occur at other places. Treatment may be with colonoscopic interventions, angiography and embolization, medication, or occasionally surgery.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and/or pancreas so they can be seen on radiographs.

Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Mallory–Weiss syndrome is a condition where high intra-abdominal pressures causes laceration and bleeding of the mucosa called Mallory-Weiss tears. Additionally, Mallory–Weiss syndrome is one of the most common causes of acute upper gastrointestinal bleeding, counting of around 1-15% of all cases in adults and less than 5% in children. It has been found that tears are up to 2 to 4 times more prevalent in men than women. The tears can cause upper gastrointestinal bleeding and predominantly occur where the esophagus meets the stomach. However, the tears can happen anywhere from the middle of the esophagus to the cardia of the stomach. Mallory–Weiss syndrome is often caused by constant vomiting and retching from alcoholism or bulimia. Gastroesophageal reflux disease (GERD) is another risk factor that is often linked with Mallory–Weiss syndrome. However, not every individual with Mallory–Weiss syndrome will have these risk factors. Individuals with Mallory–Weiss syndrome will have hematemesis, however the symptoms can vary.

Lower gastrointestinal bleeding (LGIB) is any form of gastrointestinal bleeding in the lower gastrointestinal tract. LGIB is a common reason for seeking medical attention at a hospital's emergency department. LGIB accounts for 30–40% of all gastrointestinal bleeding and is less common than upper gastrointestinal bleeding (UGIB). It is estimated that UGIB accounts for 100–200 per 100,000 cases versus 20–27 per 100,000 cases for LGIB. Approximately 85% of lower gastrointestinal bleeding involves the large intestine, 10% are from bleeds that are actually upper gastrointestinal bleeds, and 3–5% involve the small intestine.
Enteroscopy is the procedure of using an endoscope for the direct visualization of the small bowel. Etymologically, the word could potentially refer to any bowel endoscopy, but idiomatically it is conventionally restricted to small bowel endoscopy, in distinction from colonoscopy, which is large bowel endoscopy. Various types of enteroscopy exist, as follows:

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply (ischemia). Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.

Endoscopic foreign body retrieval refers to the removal of ingested objects from the esophagus, stomach and duodenum by endoscopic techniques. It does not involve surgery, but rather encompasses a variety of techniques employed through the gastroscope for grasping foreign bodies, manipulating them, and removing them while protecting the esophagus and trachea. It is of particular importance with children, people with mental illness, and prison inmates as these groups have a high rate of foreign body ingestion.

Hironori Yamamoto is a Japanese gastroenterologist and academic best known for inventing double-balloon enteroscopy (DBE), a technique that enables detailed visualization and treatment of the small intestine by endoscopy. His work has significantly advanced the field of endoluminal therapeutic endoscopy.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
Blair S. Lewis, M.D., F.A.C.P., F.A.C.G., is an American board-certified gastroenterologist and Clinical Professor of Medicine at the Mount Sinai School of Medicine. Lewis is a specialist in the field of gastrointestinal endoscopy and was the primary investigator for the first clinical trial of capsule endoscopy for the small intestine and also the first clinical trial of capsule endoscopy for the colon.

Michel Kahaleh is an American gastroenterologist and an expert in therapeutic endoscopy.
Hemostatic Powder Spray TC-325 is an inert, highly absorptive mineral agent which is used for the treatment of gastrointestinal bleeding. Applied during endoscopy to bleeding lesions, TC-325 is derived from bentonite, and is used to achieve hemostasis by absorbing water and creating a barrier that leads to mechanical tamponade (pressure) and concentration of clotting factors, resulting in enhanced coagulation. TC-325 was approved for gastrointestinal bleeding from causes other than gastric or esophageal varices. TC-325 results in immediate control of bleeding in 91-93% of cases. Technical success has gradually increased between 2011 and 2019, which may be due to device improvements or physician familiarity with the application of TC-325.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).