Varicose veins, also known as varicoses, are a medical condition in which superficial veins become enlarged and twisted. These veins typically develop in the legs, just under the skin. Varicose veins usually cause few symptoms. However, some individuals may experience fatigue or pain in the area. Complications can include bleeding or superficial thrombophlebitis. Varices in the scrotum are known as a varicocele, while those around the anus are known as hemorrhoids. Due to the various physical, social, and psychological effects of varicose veins, they can negatively affect one's quality of life.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.
The great saphenous vein (GSV) or long saphenous vein is a large, subcutaneous, superficial vein of the leg. It is the longest vein in the body, running along the length of the lower limb, returning blood from the foot, leg and thigh to the deep femoral vein at the femoral triangle.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.
Stasis dermatitis refers to the skin changes that occur in the leg as a result of "stasis" or blood pooling from insufficient venous return; the alternative name of varicose eczema comes from a common cause of this being varicose veins.

Telangiectasias, from Greek: tel- (end) + angi- + ectasia, also known as spider veins, are small dilated blood vessels that can occur near the surface of the skin or mucous membranes, measuring between 0.5 and 1 millimeter in diameter. These dilated blood vessels can develop anywhere on the body, but are commonly seen on the face around the nose, cheeks and chin. Dilated blood vessels can also develop on the legs, although when they occur on the legs, they often have underlying venous reflux or "hidden varicose veins". When found on the legs, they are found specifically on the upper thigh, below the knee joint and around the ankles.

Sclerotherapy is a procedure used to treat blood vessel malformations and also malformations of the lymphatic system. A medication is injected into the vessels, which makes them shrink. It is used for children and young adults with vascular or lymphatic malformations. In adults, sclerotherapy is often used to treat spider veins, smaller varicose veins, hemorrhoids, and hydroceles.
Polidocanol is a local anaesthetic and antipruritic component of ointments and bath additives. It relieves itching caused by eczema and dry skin. It has also been used to treat varicose veins, hemangiomas, and vascular malformations. It is formed by the ethoxylation of dodecanol.
The small saphenous vein is a relatively large superficial vein of the posterior leg.

Radiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the electrical conduction system of the heart, tumor or other dysfunctional tissue is ablated using the heat generated from medium frequency alternating current. RFA is generally conducted in the outpatient setting, using either local anesthetics or twilight anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation.
Ambulatory phlebectomy is a minisurgical treatment for superficial varicose veins and so-called side branches.
Venous cutdown is an emergency procedure in which the vein is exposed surgically and then a cannula is inserted into the vein under direct vision. It is used for venous access in cases of trauma, and hypovolemic shock when the use of a peripheral venous catheter is either difficult or impossible. The great saphenous vein is most commonly used. This procedure has fallen out of favor with the development of safer techniques for central venous catheterization such as the Seldinger technique, the modified Seldinger technique, intraosseous infusion, as well as the use of ultrasound guidance for placement of central venous catheters without using the cutdown technique.
The term venous translucence has been used in phlebology since 1996 by surgeon Pedro Fernandes Neto during ambulatory clinical exams in Brazil. His results were published in the annals of the national and international congresses of angiology. Venous translucence is the process of reflective image visualization of veins by light, which reaches up to the superficial venous system. It is a non-invasive method. Since it is a simple, low-cost technique it can be repeated as needed, which is useful in disease-process monitoring. It is a new diagnostic procedure, still undergoing investigation; more analysis is necessary to hone its technical aspects. Venous translucence is based on optical physics. It is caused by the refraction, absorption and reflection of light. The color which is not absorbed is reflected, and is the one that is seen. Therefore, venous translumination is based on the incidence of luminosity on the vein, where part of the light is absorbed and another reflected.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.

Klippel–Trénaunay syndrome, formerly Klippel–Trénaunay–Weber syndrome and sometimes angioosteohypertrophy syndrome and hemangiectatic hypertrophy, is a rare congenital medical condition in which blood vessels and/or lymph vessels fail to form properly. The three main features are nevus flammeus, venous and lymphatic malformations, and soft-tissue hypertrophy of the affected limb. It is similar to, though distinctly separate from, the less common Parkes Weber syndrome.

Paolo Zamboni is an Italian doctor and scientist. He is full Professor and Director of the School of Vascular Surgery at the University of Ferrara in Italy.

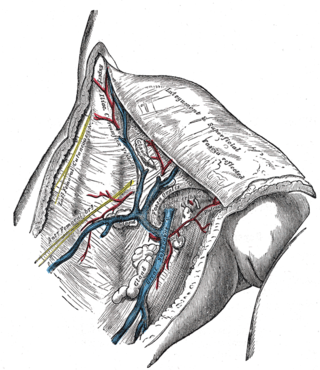
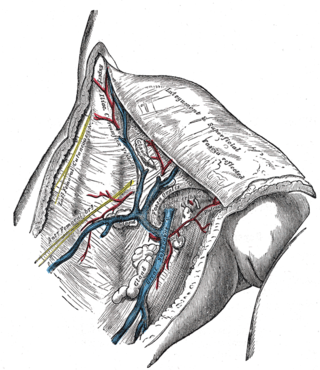
Perforator veins are so called because they perforate the deep fascia of muscles, to connect the superficial veins to the deep veins where they drain.

Ultrasonography of suspected or previously confirmed chronic venous insufficiency of leg veins is a risk-free, non-invasive procedure. It gives information about the anatomy, physiology and pathology of mainly superficial veins. As with heart ultrasound (echocardiography) studies, venous ultrasonography requires an understanding of hemodynamics in order to give useful examination reports. In chronic venous insufficiency, sonographic examination is of most benefit; in confirming varicose disease, making an assessment of the hemodynamics, and charting the progression of the disease and its response to treatment. It has become the reference standard for examining the condition and hemodynamics of the lower limb veins. Particular veins of the deep venous system (DVS), and the superficial venous system (SVS) are looked at. The great saphenous vein (GSV), and the small saphenous vein (SSV) are superficial veins which drain into respectively, the common femoral vein and the popliteal vein. These veins are deep veins. Perforator veins drain superficial veins into the deep veins. Three anatomic compartments are described, (N1) containing the deep veins, (N2) containing the perforator veins, and (N3) containing the superficial veins, known as the saphenous compartment. This compartmentalisation makes it easier for the examiner to systematize and map. The GSV can be located in the saphenous compartment where together with the Giacomini vein and the accessory saphenous vein (ASV) an image resembling an eye, known as the 'eye sign' can be seen. The ASV which is often responsible for varicose veins, can be located at the 'alignment sign', where it is seen to align with the femoral vessels.

The Giacomini vein or cranial extension of the small saphenous vein is a communicating vein between the great saphenous vein (GSV) and the small saphenous vein (SSV). It is named after the Italian anatomist Carlo Giacomini (1840–1898). The Giacomini vein courses the posterior thigh as either a trunk projection, or tributary of the SSV. In one study it was found in over two-thirds of limbs. Another study in India found the vein to be present in 92% of those examined. It is located under the superficial fascia and its insufficiency seemed of little importance in the majority of patients with varicose disease, but the use of ultrasonography has highlighted a new significance of this vein. It can be part of a draining variant of the SSV which continues on to reach the GSV at the proximal third of the thigh instead of draining into the popliteal vein. The direction of its flow is usually anterograde but it can be retrograde when this vein acts as a bypass from an insufficient GSV to SSV to call on this last one to collaborate in draining. Many discussions exist about this vein, some of them confusing to a non-expert reader. Insufficiency in the Giacomini vein can present in isolation but is mostly seen together with a GSV insufficiency. It has been shown to be effectively treated either with endovenous laser ablation or by ultrasound guided sclerotherapy.
CHIVA method is a type of surgery used to treat varicose veins that occur as a result of long term venous insufficiency. The term is a French acronym for Conservatrice Hémodynamique de l'Insuffisance Veineuse en Ambulatoire.