Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.

Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and cover of the abdominal organs. Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. One part or the entire abdomen may be tender. Complications may include shock and acute respiratory distress syndrome.

Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

Diverticulitis, also called colonic diverticulitis, is a gastrointestinal disease characterized by inflammation of abnormal pouches—diverticula—that can develop in the wall of the large intestine. Symptoms typically include lower abdominal pain of sudden onset, but the onset may also occur over a few days. There may also be nausea, diarrhea or constipation. Fever or blood in the stool suggests a complication. People may experience a single attack, repeated attacks, or ongoing "smouldering" diverticulitis.

Diverticulosis is the condition of having multiple pouches (diverticula) in the colon that are not inflamed. These are outpockets of the colonic mucosa and submucosa through weaknesses of muscle layers in the colon wall. Diverticula do not cause symptoms in most people. Diverticular disease occurs when diverticula become clinically inflamed, a condition known as diverticulitis.

Fitz-Hugh–Curtis syndrome is a rare complication of pelvic inflammatory disease (PID) involving liver capsule inflammation leading to the formation of adhesions presenting with the clinical syndrome of right upper quadrant (RUQ) pain.

A Meckel's diverticulum, a true congenital diverticulum, is a slight bulge in the small intestine present at birth and a vestigial remnant of the vitelline duct. It is the most common malformation of the gastrointestinal tract and is present in approximately 2% of the population, with males more frequently experiencing symptoms.

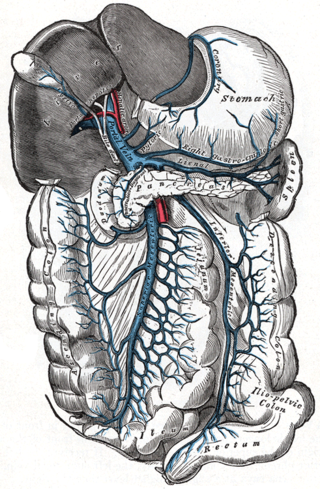
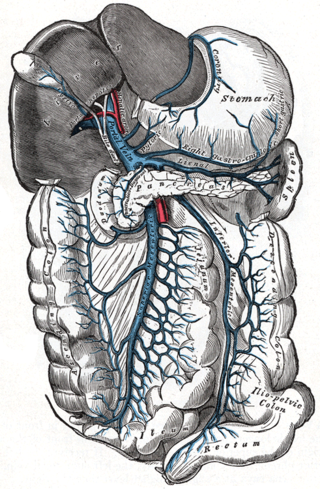
Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.

Diverticular disease is when problems occur due to diverticulosis, a benign condition defined by the formation of pouches (diverticula) from the weak spots in the wall of the large intestine. This disease spectrum includes diverticulitis, symptomatic uncomplicated diverticular disease (SUDD), and segmental colitis associated with diverticulosis (SCAD). The most common symptoms across the disease spectrum are abdominal pain and bowel habit changes such as diarrhea or constipation. Otherwise, diverticulitis presents with systemic symptoms such as fever and elevated white blood cell count whereas SUDD and SCAD don’t. Treatment ranges from conservative bowel rest to medications such as antibiotics, antispasmodics, acetaminophen, mesalamine, rifaximin, and corticosteroids depending on the specific conditions.

Gastrointestinal perforation, also known as gastrointestinal rupture, is a hole in the wall of the gastrointestinal tract. The gastrointestinal tract is composed of hollow digestive organs leading from the mouth to the anus. Symptoms of gastrointestinal perforation commonly include severe abdominal pain, nausea, and vomiting. Complications include a painful inflammation of the inner lining of the abdominal wall and sepsis.
Valentino's syndrome is pain presenting in the right lower quadrant of the abdomen caused by a duodenal ulcer with perforation through the retroperitoneum.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.
An acute abdomen refers to a sudden, severe abdominal pain. It is in many cases a medical emergency, requiring urgent and specific diagnosis. Several causes need immediate surgical treatment.
Pylephlebitis is an uncommon thrombophlebitis of the portal vein or any of its branches that is caused by infection. It is usually a complication of intra-abdominal sepsis, most often following diverticulitis, perforated appendicitis, or peritonitis. Considered uniformly lethal in the pre-antibiotic era, it still carries a mortality of 10-30%.

Omental cake is a radiologic sign indicative of an abnormally thickened greater omentum. It refers to infiltration of the normal omental structure by other types of soft-tissue or chronic inflammation resulting in a thickened, or cake-like appearance.
Abdominal guarding is the tensing of the abdominal wall muscles to guard inflamed organs within the abdomen from the pain of pressure upon them. The tensing is detected when the abdominal wall is pressed. Abdominal guarding is also known as 'défense musculaire'.

Omental infarction, or omental torsion, is an acute vascular disorder which compromises tissue of the greater omentum—the largest peritoneal fold in the abdomen.
Pelvic abscess is a collection of pus in the pelvis, typically occurring following lower abdominal surgical procedures, or as a complication of pelvic inflammatory disease (PID), appendicitis, or lower genital tract infections. Signs and symptoms include a high fever, pelvic mass, vaginal bleeding or discharge, and lower abdominal pain. It can lead to sepsis and death.