| Peritonitis | |
|---|---|
| Other names | Surgical abdomen, acute abdomen [1] |
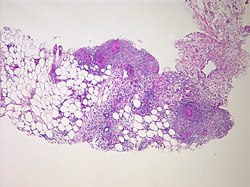 | |
| Peritonitis from tuberculosis | |
| Pronunciation | |
| Specialty | Emergency medicine, general surgery |
| Symptoms | Severe pain, swelling of the abdomen, fever [2] [3] |
| Complications | Sepsis (sepsis is likely if not quickly treated), shock, acute respiratory distress syndrome [4] [5] |
| Usual onset | Sudden [1] |
| Types | Primary, secondary, tertiary, generalized, localized [1] |
| Causes | Perforation of the intestinal tract, pancreatitis, pelvic inflammatory disease, cirrhosis, ruptured appendix [3] |
| Risk factors | Ascites, peritoneal dialysis [4] |
| Diagnostic method | Examination, blood tests, medical imaging [6] |
| Treatment | Antibiotics, intravenous fluids, pain medication, surgery [3] [4] |
| Frequency | Relatively common [1] |
Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and covering of the abdominal organs. [2] Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. [2] [3] One part or the entire abdomen may be tender. [1] Complications may include shock and acute respiratory distress syndrome. [4] [5]
Contents
- Signs and symptoms
- Abdominal pain
- Other symptoms
- Complications
- Causes
- Infection
- Non-infection
- Risk factors
- Diagnosis
- Pathology
- Treatment
- Prognosis
- Etymology
- References
- External links
Causes include perforation of the intestinal tract, pancreatitis, pelvic inflammatory disease, stomach ulcer, cirrhosis, a ruptured appendix or even a perforated gallbladder. [3] Risk factors include ascites (the abnormal build-up of fluid in the abdomen) and peritoneal dialysis. [4] Diagnosis is generally based on examination, blood tests, and medical imaging. [6]
Treatment often includes antibiotics, intravenous fluids, pain medication, and surgery. [3] [4] Other measures may include a nasogastric tube or blood transfusion. [4] Without treatment death may occur within a few days. [4] About 20% of people with cirrhosis who are hospitalized have peritonitis. [1]