Upper gastrointestinal bleeding is gastrointestinal bleeding (hemorrhage) in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.
Hematemesis is the vomiting of blood. It can be confused with hemoptysis or epistaxis (nosebleed), which are more common. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum. It may be caused by ulcers, tumors of the stomach or esophagus, varices, prolonged and vigorous retching, gastroenteritis, ingested blood, or certain drugs.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.

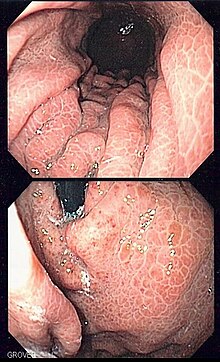
In medicine (gastroenterology), angiodysplasia is a small vascular malformation of the gut. It is a common cause of otherwise unexplained gastrointestinal bleeding and anemia. Lesions are often multiple, and frequently involve the cecum or ascending colon, although they can occur at other places. Treatment may be with colonoscopic interventions, angiography and embolization, medication, or occasionally surgery.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

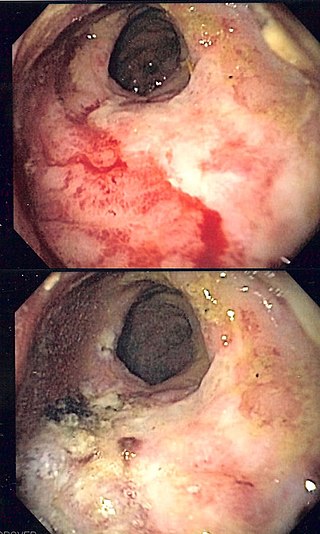
Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus. They are most often a consequence of portal hypertension, commonly due to cirrhosis. People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal. Esophageal varices are typically diagnosed through an esophagogastroduodenoscopy.
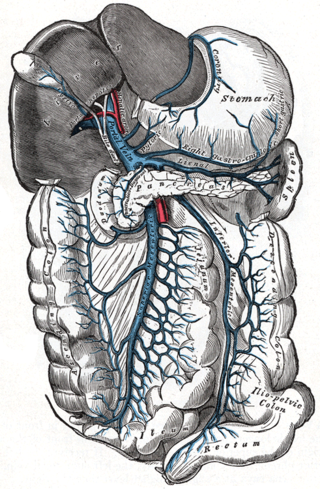
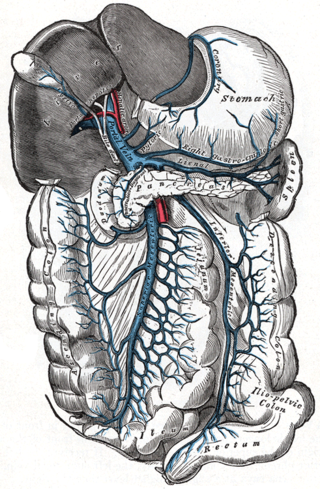
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5–9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg. The portal vein and its branches supply most of the blood and nutrients from the intestine to the liver.

Dieulafoy's lesion is a medical condition characterized by a large tortuous artery most commonly in the stomach wall (submucosal) that erodes and bleeds. It can present in any part of the gastrointestinal tract. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898. It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms, these are thought to be developmental malformations rather than degenerative changes.

Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).
Radiation proctitis or radiation proctopathy is a condition characterized by damage to the rectum after exposure to x-rays or other ionizing radiation as a part of radiation therapy. Radiation proctopathy may occur as acute inflammation called "acute radiation proctitis" or with chronic changes characterized by radiation associated vascular ectasiae (RAVE) and chronic radiation proctopathy. Radiation proctitis most commonly occurs after pelvic radiation treatment for cancers such as cervical cancer, prostate cancer, bladder cancer, and rectal cancer. RAVE and chronic radiation proctopathy involves the lower intestine, primarily the sigmoid colon and the rectum, and was previously called chronic radiation proctitis, pelvic radiation disease and radiation enteropathy.

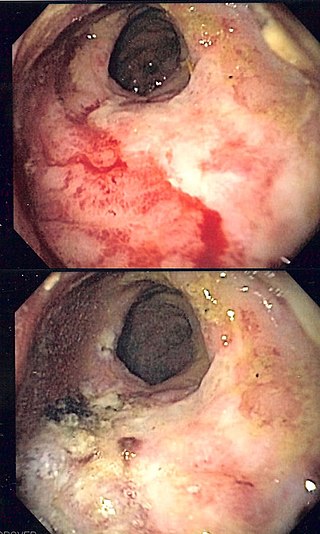
Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the pyloric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.

In medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.

Ménétrier disease is a rare, acquired, premalignant disease of the stomach characterized by massive gastric folds, excessive mucous production with resultant protein loss, and little or no acid production. The disorder is associated with excessive secretion of transforming growth factor alpha (TGF-α). It is named after a French physician Pierre Eugène Ménétrier, 1859–1935.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.
A stress ulcer is a single or multiple mucosal defect usually caused by physiological stress which can become complicated by upper gastrointestinal bleeding. These ulcers can be caused by shock, sepsis, trauma or other conditions and are found in patients with chronic illnesses. These ulcers are a significant issue in patients in critical and intensive care.

n-Butyl cyanoacrylate, a cyanoacrylate ester, is a butyl ester of 2-cyano-2-propenoic acid. It is a colorless liquid with a sharp, irritating odor. It is insoluble in water. Its chief use is as the main component of medical cyanoacrylate glues. It can be encountered under various trade names, e.g. Cutseal, MediBond, MediCryl, PeriAcryl, GluStitch, Xoin, Gesika, VetGlu, Vetbond, LiquiVet, Indermil, LiquiBand, Histoacryl, IFABond, CutisSeal and others. The generic international nonproprietary name (INN) for NBCA is enbucrilate.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.