| Bile duct | |
|---|---|
 Digestive system diagram showing the bile duct | |
 ERCP image showing the biliary tree and the main pancreatic duct. | |
| Details | |
| Identifiers | |
| Latin | ductus biliaris |
| MeSH | D001652 |
| TA98 | A05.8.02.013 A05.8.01.062 A05.8.01.065 |
| TA2 | 3103 |
| FMA | 9706 |
| Anatomical terminology | |
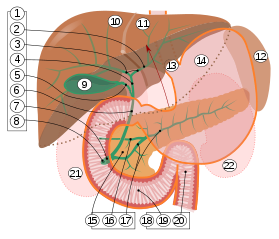
2. Intrahepatic bile ducts
3. Left and right hepatic ducts
4. Common hepatic duct
5. Cystic duct
6. Common bile duct
7. Ampulla of Vater
8. Major duodenal papilla
9. Gallbladder
10–11. Right and left lobes of liver
12. Spleen
13. Esophagus
14. Stomach
15. Pancreas :
16. Accessory pancreatic duct
17. Pancreatic duct
18. Small intestine :
19. Duodenum
20. Jejunum
21–22. Right and left kidneys
The front border of the liver has been lifted up (brown arrow).
A bile duct is any of a number of long tube-like structures that carry bile, and is present in most vertebrates. The bile duct is separated into three main parts: the fundus (superior), the body (middle), and the neck (inferior).
Contents
- Structure
- Segments
- Nerve supply
- Clinical significance
- Blockage
- Cholangiocarcinoma
- Injury
- Additional images
- References
- External links
Bile is required for the digestion of food and is secreted by the liver into passages that carry bile toward the hepatic duct. It joins the cystic duct (carrying bile to and from the gallbladder) to form the common bile duct which then opens into the intestine.





