Related Research Articles

The stomach is a muscular, hollow organ in the upper gastrointestinal tract of humans and many other animals, including several invertebrates. The stomach has a dilated structure and functions as a vital organ in the digestive system. The stomach is involved in the gastric phase of digestion, following the cephalic phase in which the sight and smell of food and the act of chewing are stimuli. In the stomach a chemical breakdown of food takes place by means of secreted digestive enzymes and gastric acid.

Peptic ulcer disease is a break in the inner lining of the stomach, the first part of the small intestine, or sometimes the lower esophagus. An ulcer in the stomach is called a gastric ulcer, while one in the first part of the intestines is a duodenal ulcer. The most common symptoms of a duodenal ulcer are waking at night with upper abdominal pain, and upper abdominal pain that improves with eating. With a gastric ulcer, the pain may worsen with eating. The pain is often described as a burning or dull ache. Other symptoms include belching, vomiting, weight loss, or poor appetite. About a third of older people with peptic ulcers have no symptoms. Complications may include bleeding, perforation, and blockage of the stomach. Bleeding occurs in as many as 15% of cases.
A hernia is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. The term is also used for the normal development of the intestinal tract, referring to the retraction of the intestine from the extra-embryonal navel coelom into the abdomen in the healthy embryo at about 7½ weeks.

Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and cover of the abdominal organs. Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. One part or the entire abdomen may be tender. Complications may include shock and acute respiratory distress syndrome.
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.

Gastric dilatation volvulus (GDV), also known as gastric dilation, twisted stomach, or gastric torsion, is a medical condition that affects dogs and rarely cats and guinea pigs, in which the stomach becomes overstretched and rotated by excessive gas content. The condition also involves compression of the diaphragm and caudal vena cavae. The word bloat is often used as a general term to mean gas distension without stomach torsion, or to refer to GDV.

The pylorus connects the stomach to the duodenum. The pylorus is considered as having two parts, the pyloric antrum and the pyloric canal. The pyloric canal ends as the pyloric orifice, which marks the junction between the stomach and the duodenum. The orifice is surrounded by a sphincter, a band of muscle, called the pyloric sphincter. The word pylorus comes from Greek πυλωρός, via Latin. The word pylorus in Greek means "gatekeeper", related to "gate" and is thus linguistically related to the word "pylon".

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".
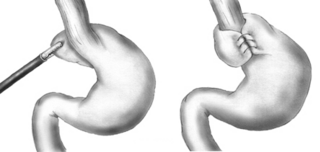
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.

Pyloric stenosis is a narrowing of the opening from the stomach to the first part of the small intestine. Symptoms include projectile vomiting without the presence of bile. This most often occurs after the baby is fed. The typical age that symptoms become obvious is two to twelve weeks old.

Dieulafoy's lesion is a medical condition characterized by a large tortuous artery most commonly in the stomach wall (submucosal) that erodes and bleeds. It can present in any part of the gastrointestinal tract. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898. It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms, these are thought to be developmental malformations rather than degenerative changes.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.
Colic in horses is defined as abdominal pain, but it is a clinical symptom rather than a diagnosis. The term colic can encompass all forms of gastrointestinal conditions which cause pain as well as other causes of abdominal pain not involving the gastrointestinal tract. What makes it tricky is that different causes can manifest with similar signs of distress in the animal. Recognizing and understanding these signs is pivotal, as timely action can spell the difference between a brief moment of discomfort and a life-threatening situation. The most common forms of colic are gastrointestinal in nature and are most often related to colonic disturbance. There are a variety of different causes of colic, some of which can prove fatal without surgical intervention. Colic surgery is usually an expensive procedure as it is major abdominal surgery, often with intensive aftercare. Among domesticated horses, colic is the leading cause of premature death. The incidence of colic in the general horse population has been estimated between 4 and 10 percent over the course of the average lifespan. Clinical signs of colic generally require treatment by a veterinarian. The conditions that cause colic can become life-threatening in a short period of time.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:
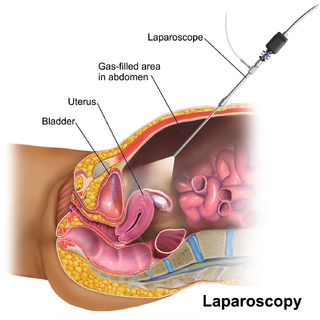
Laparoscopic hernia repair is the repair of a hiatal hernia using a laparoscope, which is a tiny telescope-like instrument. A hiatal hernia is the protrusion of an organ through its wall or cavity. There are several different methods that can be used when performing this procedure. Among them are the Nissen Fundoplication and the general laparoscopic hernia repair.

Gastric outlet obstruction (GOO) is a medical condition where there is an obstruction at the level of the pylorus, which is the outlet of the stomach. Individuals with gastric outlet obstruction will often have recurrent vomiting of food that has accumulated in the stomach, but which cannot pass into the small intestine due to the obstruction. The stomach often dilates to accommodate food intake and secretions. Causes of gastric outlet obstruction include both benign causes, such as peptic ulcer disease affecting the area around the pylorus, and malignant causes, such as gastric cancer.

Diaphragmatic rupture is a tear of the diaphragm, the muscle across the bottom of the ribcage that plays a crucial role in breathing. Most commonly, acquired diaphragmatic tears result from physical trauma. Diaphragmatic rupture can result from blunt or penetrating trauma and occurs in about 0.5% of all people with trauma.
Roemheld syndrome (RS), or gastrocardiac syndrome, or gastric cardiac syndrome or Roemheld–Techlenburg–Ceconi syndrome or gastric-cardia, was a medical syndrome first coined by Ludwig von Roemheld (1871–1938) describing a cluster of cardiovascular symptoms stimulated by gastrointestinal changes. Although it is currently considered an obsolete medical diagnosis, recent studies have described similar clinical presentations and highlighted potential underlying mechanisms.
The Sugiura procedure is a surgical technique that involves the removal and transection of the blood vessels that supply the upper portion of the stomach and the esophagus. The procedure also involves a splenectomy. The operation was originally developed to treat bleeding esophageal varices that were untreatable by other conventional methods. It was originally developed as a two-step operation, but has been modified numerous times by many surgeons since its original creation.
References
- 1 2 Carter, R; Brewer LA, 3rd; Hinshaw, DB (July 1980). "Acute gastric volvulus. A study of 25 cases". American Journal of Surgery. 140 (1): 99–106. doi:10.1016/0002-9610(80)90424-9. PMID 7396092.
{{cite journal}}: CS1 maint: numeric names: authors list (link)