An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.
Necrotizing enterocolitis (NEC) is an intestinal disease that affects premature or very low birth weight infants. Symptoms may include poor feeding, bloating, decreased activity, blood in the stool, vomiting of bile, multi-organ failure, and potentially death.
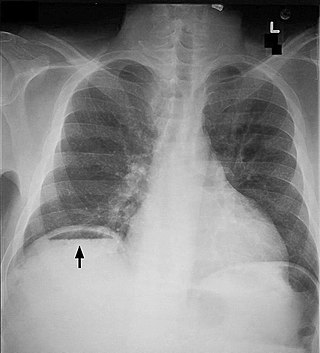
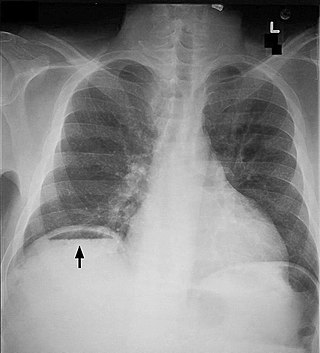
Pneumoperitoneum is pneumatosis in the peritoneal cavity, a potential space within the abdominal cavity. The most common cause is a perforated abdominal organ, generally from a perforated peptic ulcer, although any part of the bowel may perforate from a benign ulcer, tumor or abdominal trauma. A perforated appendix seldom causes a pneumoperitoneum.

Neutropenic enterocolitis, also known as typhlitis, is an inflammation of the cecum that may be associated with infection. It is particularly associated with neutropenia, a low level of neutrophil granulocytes in the blood.

Pneumomediastinum is pneumatosis in the mediastinum, the central part of the chest cavity. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. In underwater divers it is usually the result of pulmonary barotrauma.

Distal intestinal obstruction syndrome (DIOS) involves obstruction of the distal part of the small intestines by thickened intestinal content and occurs in about 20% of mainly adult individuals with cystic fibrosis. DIOS was previously known as meconium ileus equivalent, a name which highlights its similarity to the intestinal obstruction seen in newborn infants with cystic fibrosis. DIOS tends to occur in older individuals with pancreatic insufficiency. Individuals with DIOS may be predisposed to bowel obstruction, though it is a separate entity than true constipation.
Gastric volvulus or volvulus of stomach is a twisting of all or part of the stomach by more than 180 degrees with obstruction of the flow of material through the stomach, variable loss of blood supply and possible tissue death. The twisting can occur around the long axis of the stomach, called organoaxial, or around the axis perpendicular to this, called mesenteroaxial. Obstruction is more likely with organoaxial twisting than with mesenteroaxial, while the latter is more associated with ischemia. About one third of the cases are associated with a hiatal hernia. Treatment is surgical.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.

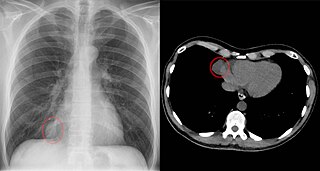
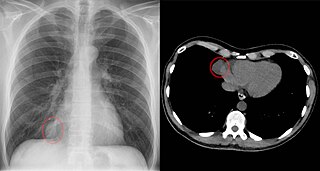
A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less than three millimetres. There may also be multiple nodules.

A pneumatocele is a cavity in the lung parenchyma filled with air that may result from pulmonary trauma during mechanical ventilation.
Cholecystostomy or (cholecystotomy) is a medical procedure used to drain the gallbladder through either a percutaneous or endoscopic approach. The procedure involves creating a stoma in the gallbladder, which can facilitate placement of a tube or stent for drainage, first performed by American surgeon, Dr. John Stough Bobbs, in 1867. It is sometimes used in cases of cholecystitis or other gallbladder disease where the person is ill, and there is a need to delay or defer cholecystectomy. The first endoscopic cholecystostomy was performed by Drs. Todd Baron and Mark Topazian in 2007 using ultrasound guidance to puncture the stomach wall and place a plastic biliary catheter for gallbladder drainage.

Computed tomography of the abdomen and pelvis is an application of computed tomography (CT) and is a sensitive method for diagnosis of abdominal diseases. It is used frequently to determine stage of cancer and to follow progress. It is also a useful test to investigate acute abdominal pain. Renal stones, appendicitis, pancreatitis, diverticulitis, abdominal aortic aneurysm, and bowel obstruction are conditions that are readily diagnosed and assessed with CT. CT is also the first line for detecting solid organ injury after trauma.

A Tornwaldt cyst is a benign cyst located in the upper posterior nasopharynx. It was first described by Gustav Ludwig Tornwaldt. It can be seen on computed tomography (CT) or magnetic resonance imaging (MRI) of the head as a well-circumscribed round mass lying in the midline. In most cases, treatment is not necessary. Indications for treatment include symptomatic lesions, large lesions (>1 cm), or lesions adjacent to the eustachian tube orifice.

Pneumatosis is the abnormal presence of air or other gas within tissues.

A lung cavity or pulmonary cavity is an abnormal, thick-walled, air-filled space within the lung. Cavities in the lung can be caused by infections, cancer, autoimmune conditions, trauma, congenital defects, or pulmonary embolism. The most common cause of a single lung cavity is lung cancer. Bacterial, mycobacterial, and fungal infections are common causes of lung cavities. Globally, tuberculosis is likely the most common infectious cause of lung cavities. Less commonly, parasitic infections can cause cavities. Viral infections almost never cause cavities. The terms cavity and cyst are frequently used interchangeably; however, a cavity is thick walled, while a cyst is thin walled. The distinction is important because cystic lesions are unlikely to be cancer, while cavitary lesions are often caused by cancer.

A focal lung pneumatosis is an enclosed pocket of air or gas in the lung and includes blebs, bullae, pulmonary cysts, and lung cavities. Blebs and bullae can be classified by their wall thickness.

Segmental colitis associated with diverticulosis (SCAD) is a condition characterized by localized inflammation in the colon, which spares the rectum and is associated with multiple sac-like protrusions or pouches in the wall of the colon (diverticulosis). Unlike diverticulitis, SCAD involves inflammation of the colon between diverticula, while sparing the diverticular orifices. SCAD may lead to abdominal pain, especially in the left lower quadrant, intermittent rectal bleeding and chronic diarrhea.
A pericardial cyst is an uncommon benign dilatation of the pericardial sac surrounding the heart. It can lead to symptoms by compressing nearby structures, but is usually asymptomatic. Pericardial cysts can be congenital or acquired, and they are typically diagnosed with radiologic imaging. Management of pericardial cysts can include follow-up imaging, percutaneous aspiration, or surgical resection.
The stepladder sign is a radiological finding observed in the context of small bowel obstruction on abdominal X-rays or computed tomography scans. It refers to the appearance of multiple, dilated small bowel loops arranged in a step-like configuration, typically visible in upright or lateral decubitus imaging positions. This sign is indicative of bowel obstruction and is used to identify and localize the site of obstruction, aiding in diagnosis and management.