A hernia is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. The term is also used for the normal development of the intestinal tract, referring to the retraction of the intestine from the extra-embryonal navel coelom into the abdomen in the healthy embryo at about 7½ weeks. Various types of hernias can occur, most commonly involving the abdomen, and specifically the groin. Groin hernias are most commonly inguinal hernias but may also be femoral hernias. Other types of hernias include hiatus, incisional, and umbilical hernias. Symptoms are present in about 66% of people with groin hernias. This may include pain or discomfort in the lower abdomen, especially with coughing, exercise, or urinating or defecating. Often, it gets worse throughout the day and improves when lying down. A bulge may appear at the site of hernia, that becomes larger when bending down. Groin hernias occur more often on the right than left side. The main concern is bowel strangulation, where the blood supply to part of the bowel is blocked. This usually produces severe pain and tenderness in the area. Hiatus, or hiatal hernias often result in heartburn but may also cause chest pain or pain while eating.

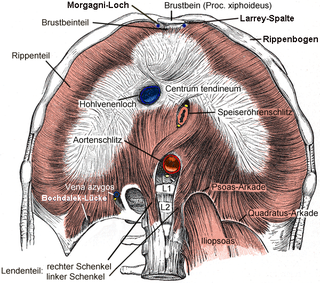
The thoracic diaphragm, or simply the diaphragm, is a sheet of internal skeletal muscle in humans and other mammals that extends across the bottom of the thoracic cavity. The diaphragm is the most important muscle of respiration, and separates the thoracic cavity, containing the heart and lungs, from the abdominal cavity: as the diaphragm contracts, the volume of the thoracic cavity increases, creating a negative pressure there, which draws air into the lungs. Its high oxygen consumption is noted by the many mitochondria and capillaries present; more than in any other skeletal muscle.

Omphalocele or omphalocoele also called exomphalos, is a rare abdominal wall defect. Beginning at the 6th week of development, rapid elongation of the gut and increased liver size reduces intra abdominal space, which pushes intestinal loops out of the abdominal cavity. Around 10th week, the intestine returns to the abdominal cavity and the process is completed by the 12th week. Persistence of intestine or the presence of other abdominal viscera in the umbilical cord results in an omphalocele.

Polyhydramnios is a medical condition describing an excess of amniotic fluid in the amniotic sac. It is seen in about 1% of pregnancies. It is typically diagnosed when the amniotic fluid index (AFI) is greater than 24 cm. There are two clinical varieties of polyhydramnios: chronic polyhydramnios where excess amniotic fluid accumulates gradually, and acute polyhydramnios where excess amniotic fluid collects rapidly.

A pulmonary sequestration is a medical condition wherein a piece of tissue that ultimately develops into lung tissue is not attached to the pulmonary arterial blood supply, as is the case in normally developing lung. This sequestered tissue is therefore not connected to the normal bronchial airway architecture, and fails to function in, and contribute to, respiration of the organism.

Vincent Alexander Bochdalek was a Bohemian anatomist and pathologist. His first name has also been given as Vincenc and Vincenz. Bochdalek was elected as member of the German Academy of Sciences Leopoldina.

Scimitar syndrome, or congenital pulmonary venolobar syndrome, is a rare congenital heart defect characterized by anomalous venous return from the right lung. This anomalous pulmonary venous return can be either partial (PAPVR) or total (TAPVR). The syndrome associated with PAPVR is more commonly known as Scimitar syndrome after the curvilinear pattern created on a chest radiograph by the pulmonary veins that drain to the inferior vena cava. This radiographic density often has the shape of a scimitar, a type of curved sword. The syndrome was first described by Catherine Neill in 1960.

Diaphragmatic hernia is a defect or hole in the diaphragm that allows the abdominal contents to move into the chest cavity. Treatment is usually surgical.

Catamenial pneumothorax is a spontaneous pneumothorax that recurs during menstruation, within 72 hours before or after the onset of a cycle. It usually involves the right side of the chest and right lung, and is associated with thoracic endometriosis. A third to a half of patients have pelvic endometriosis as well. Despite this association, CP is still considered to be misunderstood as is endometriosis considered to be underdiagnosed. The lack of a clear cause means that diagnosis and treatment is difficult. The disease is believed to be largely undiagnosed or misdiagnosed, leaving the true frequency unknown in the general population.

Pentalogy of Cantrell is an extremely rare congenital syndrome that causes defects involving the diaphragm, abdominal wall, pericardium, heart and lower sternum.
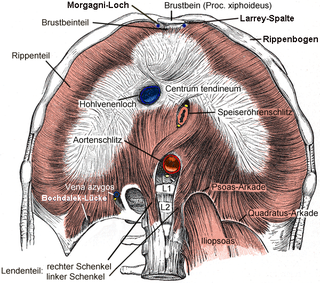
Bochdalek hernia is one of two forms of a congenital diaphragmatic hernia, the other form being Morgagni hernia. A Bochdalek hernia is a congenital abnormality in which an opening exists in the infant's diaphragm, allowing normally intra-abdominal organs to enter into the thoracic cavity. In the majority of people, the affected lung will be deformed, and the resulting lung compression can be life-threatening. Bochdalek hernias occur more commonly on the posterior left side.

Zinc finger protein ZFPM2, i.e. zinc finger protein, FOG family member 2, but also termed Friend of GATA2, Friend of GATA-2, FOG2, or FOG-2, is a protein that in humans is encoded by the ZFPM2 and in mice by the Zfpm2 gene.

Diaphragmatic rupture is a tear of the diaphragm, the muscle across the bottom of the ribcage that plays a crucial role in breathing. Most commonly, acquired diaphragmatic tears result from physical trauma. Diaphragmatic rupture can result from blunt or penetrating trauma and occurs in about 0.5% of all people with trauma.

Pulmonary hypoplasia is incomplete development of the lungs, resulting in an abnormally low number or small size of bronchopulmonary segments or alveoli. A congenital malformation, it most often occurs secondary to other fetal abnormalities that interfere with normal development of the lungs. Primary (idiopathic) pulmonary hypoplasia is rare and usually not associated with other maternal or fetal abnormalities.

Fryns syndrome is an autosomal recessive multiple congenital anomaly syndrome that is usually lethal in the neonatal period. Fryns (1987) reviewed the syndrome.

Donnai–Barrow syndrome is a genetic disorder first described by Dian Donnai and Margaret Barrow in 1993. It is associated with LRP2. It is an inherited (genetic) disorder that affects many parts of the body.
Abdominal wall defects are a type of congenital defect that allows the stomach, the intestines, or other organs to protrude through an unusual opening that forms on the abdomen.
Lung hernia is a protrusion of lung outside of thoracic wall. In 20% patients with lung hernia, the incidence is congenital. In 80% of the cases, the hernia is noted after chest trauma, thoracic surgery or certain pulmonary diseases. Congenital hernia occurs because of the weakness of the suprapleural membrane or neck muscles. In pulmonary diseases such as asthma, frequent coughing can lead to high intra thoracic pressure, causing the lung to herniate out. Lung hernia may occur near the neck (cervical), between the ribs (intercostal), near the vertebrae (paravertebral) or near the sternum (parasternal).

Pulmonary agenesis is an inborn lung underdevelopment that is rare and potentially lethal. The disorder is caused by a complete developmental arrest of the primitive lung during embryonic life, and it is often associated with other developmental defects. Bilateral and unilateral pulmonary agenesis are classified, depending on whether one side of the lung or both sides are affected. Bilateral pulmonary agenesis is lethal, while the mortality rate of unilateral pulmonary agenesis is higher than 50%. Depending on the severity, the symptom ranges from none to various respiratory complaints. It is detectable prenatally, however, its nonspecific clinical features act as the obstacle for diagnosing. The exact cause of pulmonary agenesis is still obscure. However, theories have been raised regarding the vascular, iatrogenic, viral and genetic causes of pulmonary agenesis in an attempt to explain the pathogenesis of the disorder. In most cases of pulmonary agenesis, surgical resection is performed to remove the malformed lobe or the entire defected lung of the patient depending on the severity of the respiratory impairment.
Meacham syndrome is a rare genetic disorder which is characterized by lung, diaphragmatic and genitourinary anomalies.