DNA damage
One general mechanism, increased DNA damage, is shared by some of the major liver diseases, including infection by hepatitis B virus or hepatitis C virus , heavy alcohol consumption, and obesity. [24]
Viral infection by hepatitis B virus, or hepatitis C virus causes an increase of reactive oxygen species. The increase in intracellular reactive oxygen species is about 10,000-fold with chronic hepatitis B virus infection and 100,000-fold following hepatitis C virus infection. [25] This increase in reactive oxygen species causes inflammation [25] and more than 20 types of DNA damage. [26] Oxidative DNA damage is mutagenic [27] and also causes epigenetic alterations at the sites of DNA repair. [28] Epigenetic alterations and mutations affect the cellular machinery that may cause the cell to replicate at a higher rate or result in the cell avoiding apoptosis, and thus contribute to liver disease. [29] By the time accumulating epigenetic and mutational changes eventually cause hepatocellular carcinoma, epigenetic alterations appear to have an even larger role in carcinogenesis than mutations. Only one gene, TP53, is mutated in more than 20% of liver cancers while 41 genes each have hypermethylated promoters (repressing gene expression) in more than 20% of liver cancers. [30]
Alcohol consumption in excess causes a build-up of acetaldehyde. Acetaldehyde and free radicals generated by metabolizing alcohol induce DNA damage and oxidative stress. [31] [32] [33] In addition, activation of neutrophils in alcoholic liver disease contributes to the pathogenesis of hepatocellular damage by releasing reactive oxygen species (which can damage DNA). [34] The level of oxidative stress and acetaldehyde-induced DNA adducts due to alcohol consumption does not appear sufficient to cause increased mutagenesis. [34] However, as reviewed by Nishida et al., [28] alcohol exposure, causing oxidative DNA damage (which is repairable), can result in epigenetic alterations at the sites of DNA repair. Alcohol-induced epigenetic alterations of gene expression appear to lead to liver injury and ultimately carcinoma. [35]
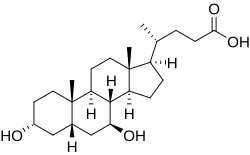
Obesity is associated with a higher risk of primary liver cancer. [36] As shown with mice, obese mice are prone to liver cancer, likely due to two factors. Obese mice have increased pro-inflammatory cytokines. Obese mice also have higher levels of deoxycholic acid, a product of bile acid alteration by certain gut microbes, and these microbes are increased with obesity. The excess deoxycholic acid causes DNA damage and inflammation in the liver, which, in turn, can lead to liver cancer. [37]
Other relevant aspects
Several liver diseases are due to viral infection. Viral hepatitides such as Hepatitis B virus and Hepatitis C virus can be vertically transmitted during birth via contact with infected blood. [38] [39] According to a 2012 NICE publication, "about 85% of hepatitis B infections in newborns become chronic". [40] In occult cases, Hepatitis B virus is present by hepatitis B virus DNA, but testing for HBsAg is negative. [41] High consumption of alcohol can lead to several forms of liver disease including alcoholic hepatitis, alcoholic fatty liver disease, cirrhosis, and liver cancer. [42] In the earlier stages of alcoholic liver disease, fat builds up in the liver's cells due to increased creation of triglycerides and fatty acids and a decreased ability to break down fatty acids. [43] Progression of the disease can lead to liver inflammation from the excess fat in the liver. Scarring in the liver often occurs as the body attempts to heal and extensive scarring can lead to the development of cirrhosis in more advanced stages of the disease. [43] Approximately 3–10% of individuals with cirrhosis develop a form of liver cancer known as hepatocellular carcinoma. [43] According to Tilg, et al., gut microbiome could very well have an effect, be involved in the pathophysiology, on the various types of liver disease which an individual may encounter. [44] Insight into the exact causes and mechanisms mediating pathophysiology of the liver is quickly progressing due to the introduction new technological approaches like Single cell sequencing and kinome profiling [45]
Air pollutants
Particulate matter or carbon black are common pollutants. They have a direct toxic effect on the liver; cause inflammation of liver caused by and thereby impact lipid metabolism and fatty liver disease; and can translocate from the lungs to the liver. [46]
Because particulate matter and carbon black are very diverse and each has different toxicodynamics, detailed mechanisms of translocation are not clear. Water-soluble fractions of particulate matter are the most important part of translocation to the liver, through extrapulmonary circulation. When particulate matter gets into the bloodstream, it combines with immune cells and stimulates innate immune responses. Pro-inflammatory cytokines are released and cause disease progression. [46]