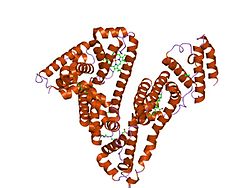
1ao6: CRYSTAL STRUCTURE OF HUMAN SERUM ALBUMIN
1bj5: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTIC ACID
1bke: HUMAN SERUM ALBUMIN IN A COMPLEX WITH MYRISTIC ACID AND TRI-IODOBENZOIC ACID
1bm0: CRYSTAL STRUCTURE OF HUMAN SERUM ALBUMIN
1e78: CRYSTAL STRUCTURE OF HUMAN SERUM ALBUMIN
1e7a: CRYSTAL STRUCTURE OF HUMAN SERUM ALBUMIN COMPLEXED WITH THE GENERAL ANESTHETIC PROPOFOL
1e7b: CRYSTAL STRUCTURE OF HUMAN SERUM ALBUMIN COMPLEXED WITH THE GENERAL ANESTHETIC HALOTHANE
1e7c: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTIC ACID AND THE GENERAL ANESTHETIC HALOTHANE
1e7e: HUMAN SERUM ALBUMIN COMPLEXED WITH DECANOIC ACID (CAPRIC ACID)
1e7f: HUMAN SERUM ALBUMIN COMPLEXED WITH DODECANOIC ACID (LAURIC ACID)
1e7g: HUMAN SERUM ALBUMIN COMPLEXED WITH TETRADECANOIC ACID (MYRISTIC ACID) HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTIC ACID
1e7h: HUMAN SERUM ALBUMIN COMPLEXED WITH HEXADECANOIC ACID (PALMITIC ACID)
1e7i: HUMAN SERUM ALBUMIN COMPLEXED WITH OCTADECANOIC ACID (STEARIC ACID)
1gni: HUMAN SERUM ALBUMIN COMPLEXED WITH CIS-9-OCTADECENOIC ACID (OLEIC ACID)
1gnj: HUMAN SERUM ALBUMIN COMPLEXED WITH CIS-5,8,11,14-EICOSATETRAENOIC ACID (ARACHIDONIC ACID)
1h9z: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTIC ACID AND THE R-(+) ENANTIOMER OF WARFARIN
1ha2: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTIC ACID AND THE S-(-) ENANTIOMER OF WARFARIN
1hk1: HUMAN SERUM ALBUMIN COMPLEXED WITH THYROXINE (3,3',5,5'-TETRAIODO-L-THYRONINE)
1hk2: HUMAN SERUM ALBUMIN MUTANT R218H COMPLEXED WITH THYROXINE (3,3',5,5'-TETRAIODO-L-THYRONINE)
1hk3: HUMAN SERUM ALBUMIN MUTANT R218P COMPLEXED WITH THYROXINE (3,3',5,5'-TETRAIODO-L-THYRONINE)
1hk4: HUMAN SERUM ALBUMIN COMPLEXED WITH THYROXINE (3,3',5,5'-TETRAIODO-L-THYRONINE) AND MYRISTIC ACID (TETRADECANOIC ACID)
1hk5: HUMAN SERUM ALBUMIN MUTANT R218H COMPLEXED WITH THYROXINE (3,3',5,5'-TETRAIODO-L-THYRONINE) AND MYRISTIC ACID (TETRADECANOIC ACID)
1n5u: X-RAY STUDY OF HUMAN SERUM ALBUMIN COMPLEXED WITH HEME
1o9x: HUMAN SERUM ALBUMIN COMPLEXED WITH TETRADECANOIC ACID (MYRISTIC ACID) AND HEMIN
1tf0: Crystal structure of the GA module complexed with human serum albumin
1uor: X-RAY STUDY OF RECOMBINANT HUMAN SERUM ALBUMIN. PHASES DETERMINED BY MOLECULAR REPLACEMENT METHOD, USING LOW RESOLUTION STRUCTURE MODEL OF TETRAGONAL FORM OF HUMAN SERUM ALBUMIN
1ysx: Solution structure of domain 3 from human serum albumin complexed to an anti-apoptotic ligand directed against Bcl-xL and Bcl-2
2bx8: HUMAN SERUM ALBUMIN COMPLEXED WITH AZAPROPAZONE
2bxa: HUMAN SERUM ALBUMIN COMPLEXED WITH 3-CARBOXY-4-METHYL-5-PROPYL-2-FURANPROPANOIC ACID (CMPF)
2bxb: HUMAN SERUM ALBUMIN COMPLEXED WITH OXYPHENBUTAZONE
2bxc: HUMAN SERUM ALBUMIN COMPLEXED WITH PHENYLBUTAZONE
2bxd: HUMAN SERUM ALBUMIN COMPLEXED WITH WARFARIN
2bxe: HUMAN SERUM ALBUMIN COMPLEXED WITH DIFLUNISAL
2bxf: HUMAN SERUM ALBUMIN COMPLEXED WITH DIAZEPAM
2bxg: HUMAN SERUM ALBUMIN COMPLEXED WITH IBUPROFEN
2bxh: HUMAN SERUM ALBUMIN COMPLEXED WITH INDOXYL SULFATE
2bxi: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND AZAPROPAZONE
2bxk: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE, AZAPROPAZONE AND INDOMETHACIN
2bxl: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND 3,5-DIIODOSALICYLIC ACID
2bxm: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND INDOMETHACIN
2bxn: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND IODIPAMIDE
2bxo: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND OXYPHENBUTAZONE
2bxp: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE AND PHENYLBUTAZONE
2bxq: HUMAN SERUM ALBUMIN COMPLEXED WITH MYRISTATE, PHENYLBUTAZONE AND INDOMETHACIN
2i2z: Human serum albumin complexed with myristate and aspirin
2i30: Human serum albumin complexed with myristate and salicylic acid