Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

Edema, also spelled oedema, and also known as fluid retention, dropsy and hydropsy, is the build-up of fluid in the body's tissue, a type of swelling. Most commonly, the legs or arms are affected. Symptoms may include skin that feels tight, the area feeling heavy, and joint stiffness. Other symptoms depend on the underlying cause.

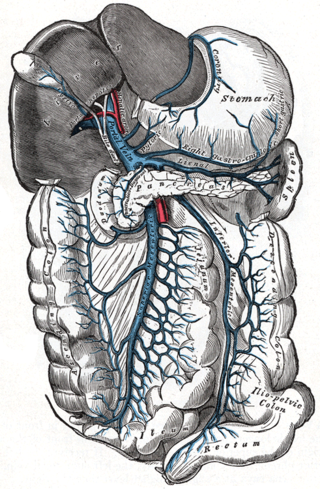
The portal vein or hepatic portal vein (HPV) is a blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas and spleen to the liver. This blood contains nutrients and toxins extracted from digested contents. Approximately 75% of total liver blood flow is through the portal vein, with the remainder coming from the hepatic artery proper. The blood leaves the liver to the heart in the hepatic veins.

Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood.
Pulmonary heart disease, also known as cor pulmonale, is the enlargement and failure of the right ventricle of the heart as a response to increased vascular resistance or high blood pressure in the lungs.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.
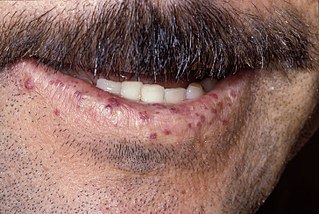
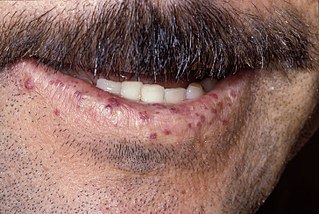
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.
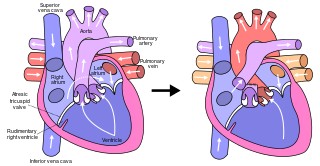
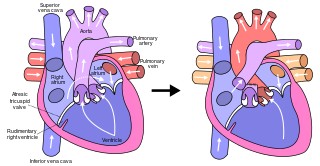
The Fontan procedure or Fontan–Kreutzer procedure is a palliative surgical procedure used in children with univentricular hearts. It involves diverting the venous blood from the inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries. The procedure varies for differing congenital heart pathologies. For example, in tricuspid atresia, the procedure can be done where the blood does not pass through the morphologic right ventricle; i.e., the systemic and pulmonary circulations are placed in series with the functional single ventricle. By contrast, in hypoplastic left heart syndrome, the heart is more reliant on the more functional right ventricle to provide blood flow to the systemic circulation. The procedure was initially performed in 1968 by Francis Fontan and Eugene Baudet from Bordeaux, France, published in 1971, simultaneously described in July 1971 by Guillermo Kreutzer from Buenos Aires, Argentina, presented at the Argentinean National Cardilogy meeting of that year and finally published in 1973.

In human anatomy, the hepatic veins are the veins that drain venous blood from the liver into the inferior vena cava. There are usually three large upper hepatic veins draining from the left, middle, and right parts of the liver, as well as a number (6-20) of lower hepatic veins. All hepatic veins are valveless.

Inferior vena cava syndrome (IVCS) is a very rare constellation of symptoms resulting from either obstruction or stenosis of the inferior vena cava. It can be caused by physical invasion or compression by a pathological process, or by thrombosis within the vein itself. It can also occur during pregnancy. Symptoms including high venous pressure in the lower limbs, decreased blood return to the heart, decreased cardiac output, placental separation and decreased kidney function have been observed in late term pregnancy. Studies show that all of these issues can arise from lying in the supine position during late pregnancy, which can cause compression and obstruction of the inferior vena cava by the uterus. Symptoms of late pregnancy inferior vena cava syndrome consist of intense pain in the right hand side, muscle twitching, hypotension, and fluid retention.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).
Cardiac asthma is the medical condition of intermittent wheezing, coughing, and shortness of breath that is associated with underlying congestive heart failure (CHF). Symptoms of cardiac asthma are related to the heart's inability to effectively and efficiently pump blood in a CHF patient. This can lead to accumulation of fluid in and around the lungs, disrupting the lung's ability to oxygenate blood.

Portal vein thrombosis (PVT) is a vascular disease of the liver that occurs when a blood clot occurs in the hepatic portal vein, which can lead to increased pressure in the portal vein system and reduced blood supply to the liver. The mortality rate is approximately 1 in 10.
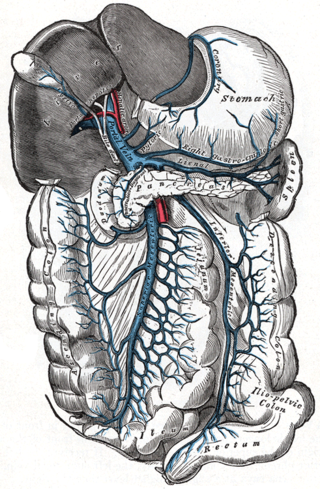
In human anatomy, the hepatic portal system or portal venous system is the system of veins comprising the portal vein and its tributaries. The other portal venous system in the body is the hypophyseal portal system.
Collateral circulation is the alternate circulation around a blocked artery or vein via another path, such as nearby minor vessels. It may occur via preexisting vascular redundancy, as in the circle of Willis in the brain, or it may occur via new branches formed between adjacent blood vessels (neovascularization), as in the eye after a retinal embolism or in the brain when an instance of arterial constriction occurs due to Moyamoya disease. Its formation may be related by pathological conditions such as high vascular resistance or ischaemia. It is occasionally also known as accessory circulation, auxiliary circulation, or secondary circulation. It has surgically created analogues in which shunts or anastomoses are constructed to bypass circulatory problems.
Hepatic veno-occlusive disease (VOD) or veno-occlusive disease with immunodeficiency is a potentially life-threatening condition in which some of the small veins in the liver are obstructed. It is a complication of high-dose chemotherapy given before a bone marrow transplant and/or excessive exposure to hepatotoxic pyrrolizidine alkaloids. It is classically marked by weight gain due to fluid retention, increased liver size, and raised levels of bilirubin in the blood. The name sinusoidal obstruction syndrome (SOS) is preferred if hepatic veno-occlusive disease happens as a result of chemotherapy or bone marrow transplantation.

Ischemic hepatitis, also known as shock liver, is a condition defined as an acute liver injury caused by insufficient blood flow to the liver. The decreased blood flow (perfusion) to the liver is usually due to shock or low blood pressure. However, local causes involving the hepatic artery that supplies oxygen to the liver, such as a blood clot in the hepatic artery, can also cause ischemic hepatitis.

The liver is a major metabolic organ exclusively found in vertebrate animals, which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and various other biochemicals necessary for digestion and growth. In humans, it is located in the right upper quadrant of the abdomen, below the diaphragm and mostly shielded by the lower right rib cage. Its other metabolic roles include carbohydrate metabolism, the production of hormones, conversion and storage of nutrients such as glucose and glycogen, and the decomposition of red blood cells.

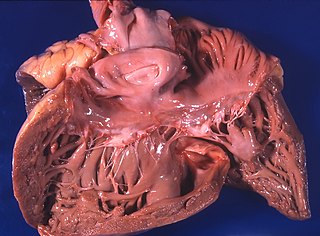
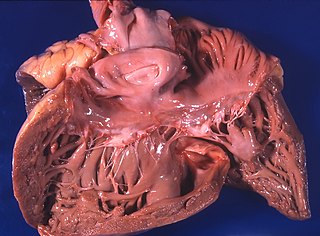
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, chronic liver failure or chronic hepatic failure and end-stage liver disease, is a condition of the liver in which the normal functioning tissue, or parenchyma, is replaced with scar tissue (fibrosis) and regenerative nodules as a result of chronic liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue and nodules of regenerating hepatocytes can replace the parenchyma, causing increased resistance to blood flow in the liver's capillaries—the hepatic sinusoids—and consequently portal hypertension, as well as impairment in other aspects of liver function. The disease typically develops slowly over months or years.