The term abdominal surgery broadly covers surgical procedures that involve opening the abdomen (laparotomy). Surgery of each abdominal organ is dealt with separately in connection with the description of that organ Diseases affecting the abdominal cavity are dealt with generally under their own names.

General surgery is a surgical specialty that focuses on alimentary canal and abdominal contents including the esophagus, stomach, small intestine, large intestine, liver, pancreas, gallbladder, appendix and bile ducts, and often the thyroid gland. General surgeons also deal with diseases involving the skin, breast, soft tissue, trauma, peripheral artery disease and hernias and perform endoscopic as such as gastroscopy, colonoscopy and laparoscopic procedures.

Surgery is a medical specialty that uses manual and instrumental techniques to diagnose or treat pathological conditions, to alter bodily functions, to reconstruct or improve aesthetics and appearance, or to remove unwanted tissues or foreign bodies.
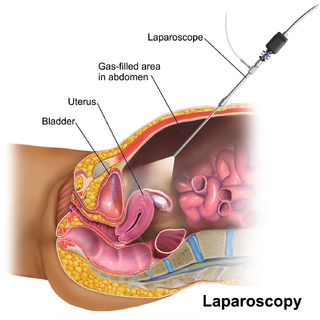
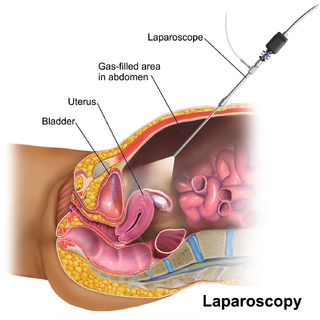
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.

An appendectomy or appendicectomy is a surgical operation in which the vermiform appendix is removed. Appendectomy is normally performed as an urgent or emergency procedure to treat complicated acute appendicitis.
A trauma center, or trauma centre, is a hospital equipped and staffed to provide care for patients suffering from major traumatic injuries such as falls, motor vehicle collisions, or gunshot wounds. A trauma center may also refer to an emergency department without the presence of specialized services to care for victims of major trauma.
A laparotomy is a surgical procedure involving a surgical incision through the abdominal wall to gain access into the abdominal cavity. It is also known as a celiotomy.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

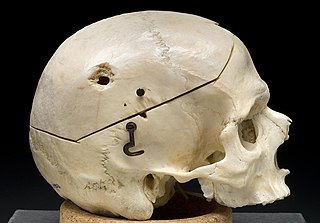
Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, and sports-related injuries, and are notably common among the elderly who experience falls.
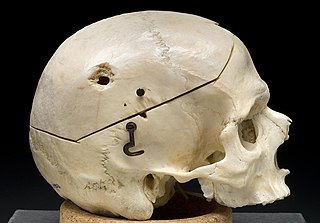
A gunshot wound (GSW) is a penetrating injury caused by a projectile shot from a gun. Damage may include bleeding, bone fractures, organ damage, wound infection, and loss of the ability to move part of the body. Damage depends on the part of the body hit, the path the bullet follows through the body, and the type and speed of the bullet. In severe cases, although not uncommon, the injury is fatal. Long-term complications can include bowel obstruction, failure to thrive, neurogenic bladder and paralysis, recurrent cardiorespiratory distress and pneumothorax, hypoxic brain injury leading to early dementia, amputations, chronic pain and pain with light touch (hyperalgesia), deep venous thrombosis with pulmonary embolus, limb swelling and debility, and lead poisoning.

Penetrating trauma is an open wound injury that occurs when an object pierces the skin and enters a tissue of the body, creating a deep but relatively narrow entry wound. In contrast, a blunt or non-penetrating trauma may have some deep damage, but the overlying skin is not necessarily broken and the wound is still closed to the outside environment. The penetrating object may remain in the tissues, come back out the path it entered, or pass through the full thickness of the tissues and exit from another area.

Lincoln Hospital is a full service medical center and teaching hospital affiliated with Weill Cornell Medical College, in the Mott Haven neighborhood of the Bronx, New York City, New York. The medical center is municipally owned by NYC Health + Hospitals.

Abdominal trauma is an injury to the abdomen. Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Complications may include blood loss and infection.
An exploratory laparotomy is a general surgical operation where the abdomen is opened and the abdominal organs are examined for injury or disease. It is the standard of care in various blunt and penetrating trauma situations in which there may be life-threatening internal injuries. It is also used in certain diagnostic situations, in which the operation is undertaken in search of a unifying cause for multiple signs and symptoms of disease, and in the staging of some cancers.
Dietmar H. Wittmann is a German academic surgeon specializing in complex abdominal surgery. He was associated with the following medical schools: University of Hamburg, Germany, University of Düsseldorf, Germany, University of California San Francisco Medical School,USA, Hahnemann Medical School, Philadelphia,USA, Medical College of Wisconsin Milwaukee, USA. In addition to his clinical work, research, publications and teaching and lecturing worldwide, he is mostly known for his work relating to intra-abdominal infections, abdominal compartment syndrome abdominal compartment syndrome and staged abdominal repair STAR. Besides introducing the concept of calculated antimicrobial therapy Wittmann conceptualized the operative strategy of Staged Abdominal Repair (STAR) or the planned open abdomen to reverse the detrimental effects of the abdominal compartment syndrome and to treat imminent intra abdominal complications before they progress to life-threatening conditions. He is the inventor of a fascia prosthesis for temporary abdominal closure, the Artificial Bur Fascia Prosthesis (generic) or Wittmann Patch and Star Patch.

George Emory Goodfellow was a physician and naturalist in the 19th- and early 20th-century American Old West who developed a reputation as the United States' foremost expert in treating gunshot wounds. As a medical practitioner in Tombstone, Arizona Territory, Goodfellow treated numerous bullet wounds to both lawmen and outlaws. He recorded several significant medical firsts throughout his career, including performing the first documented laparotomy for treating an abdominal gunshot wound and the first perineal prostatectomy to remove an enlarged prostate. He also pioneered the use of spinal anesthesia and sterile techniques in treating gunshot wounds and is regarded as the first civilian trauma surgeon.

A stab wound is a specific form of penetrating trauma to the skin that results from a knife or a similar pointed object. While stab wounds are typically known to be caused by knives, they can also occur from a variety of implements, including broken bottles and ice picks. Most stabbings occur because of intentional violence or through self-infliction. The treatment is dependent on many different variables such as the anatomical location and the severity of the injury. Even though stab wounds are inflicted at a much greater rate than gunshot wounds, they account for less than 10% of all penetrating trauma deaths.
A pancreatic injury is some form of trauma sustained by the pancreas. The injury can be sustained through either blunt forces, such as a motor vehicle accident, or penetrative forces, such as that of a gunshot wound. The pancreas is one of the least commonly injured organs in abdominal trauma.
Damage control surgery is surgical intervention to keep the patient alive rather than correct the anatomy. It addresses the "lethal triad" for critically ill patients with severe hemorrhage affecting homeostasis leading to metabolic acidosis, hypothermia, and increased coagulopathy.

The 274th Forward Surgical Team (Airborne)—part of the 274th Forward Resuscitative and Surgical Detachment (Airborne)—is an airborne forward surgical team of the United States Army providing Level II care far forward on the battlefield. It was first constituted in 1944 and served in Europe during World War II. More recently it has been involved in relief operations following natural disasters and has undertaken several recent deployments to Iraq and Afghanistan. The 274th Forward Surgical Team was part of both the initial entry forces of Operation Enduring Freedom in 2001 and Operation Iraqi Freedom in 2003. Currently the unit falls under the command of the 28th Combat Support Hospital and is based at Fort Bragg, North Carolina.