A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened, fails to respond normally to painful stimuli, light, or sound, lacks a normal wake-sleep cycle and does not initiate voluntary actions. The person may experience respiratory and circulatory problems due to the body's inability to maintain normal bodily functions. People in a coma often require extensive medical care to maintain their health and prevent complications such as pneumonia or blood clots. Coma patients exhibit a complete absence of wakefulness and are unable to consciously feel, speak or move. Comas can be derived by natural causes, or can be medically induced.
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.
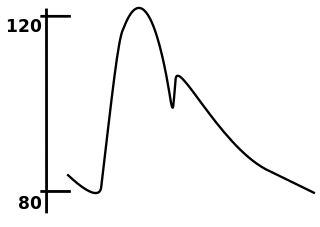
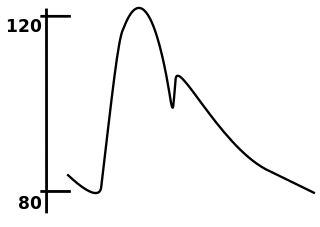
In medicine, the mean arterial pressure (MAP) is an average calculated blood pressure in an individual during a single cardiac cycle. Although methods of estimating MAP vary, a common calculation is to take one-third of the pulse pressure, and add that amount to the diastolic pressure. A normal MAP is about 90 mmHg.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.
APACHE II is a severity-of-disease classification system, one of several ICU scoring systems. It is applied within 24 hours of admission of a patient to an intensive care unit (ICU): an integer score from 0 to 71 is computed based on several measurements; higher scores correspond to more severe disease and a higher risk of death. The first APACHE model was presented by Knaus et al. in 1981.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.

Vital signs are a group of the four to six most crucial medical signs that indicate the status of the body's vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person's vital signs vary with age, weight, sex, and overall health.
Abnormal posturing is an involuntary flexion or extension of the arms and legs, indicating severe brain injury. It occurs when one set of muscles becomes incapacitated while the opposing set is not, and an external stimulus such as pain causes the working set of muscles to contract. The posturing may also occur without a stimulus. Since posturing is an important indicator of the amount of damage that has occurred to the brain, it is used by medical professionals to measure the severity of a coma with the Glasgow Coma Scale and the Pediatric Glasgow Coma Scale.

Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause blanching. It can be measured by holding a hand higher than heart-level and pressing the soft pad of a finger or fingernail until it turns white, then taking note of the time needed for the color to return once pressure is released. In humans, CRT of more than three seconds indicates decreased peripheral perfusion and may indicate cardiovascular or respiratory dysfunction. The most reliable and applicable site for CRT testing is the finger pulp, and the cut-off value for the normal CRT should be 3 seconds, not 2 seconds.
SAPS II is a severity of disease classification system. Its name stands for "Simplified Acute Physiology Score", and is one of several ICU scoring systems.
The Simplified Acute Physiology Score III is a system for predicting mortality, one of several ICU scoring systems. It is a supplement to the SAPS II scoring system. It has been designed to provide a real-life predicted mortality for a patient by following a well defined procedure, based on a mathematical model that needs calibration. Predicted mortalities are good when comparing groups of patients, and having near-real-life mortalities means, that this scoring system can answer questions like "if the patients from hospital A had been in hospital B, what would their mortality have been?".

Fat embolism syndrome occurs when fat enters the blood stream and results in symptoms. Symptoms generally begin within a day. This may include a petechial rash, decreased level of consciousness, and shortness of breath. Other symptoms may include fever and decreased urine output. The risk of death is about 10%.
The Injury Severity Score (ISS) is an established medical score to assess trauma severity. It correlates with mortality, morbidity and hospitalization time after trauma. It is used to define the term major trauma. A major trauma is defined as the Injury Severity Score being greater than 15. The AIS Committee of the Association for the Advancement of Automotive Medicine (AAAM) designed and improves upon the scale.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.
Blunt trauma personal protective equipment (PPE) protects the wearer against injuries caused by blunt impacts. For law enforcement, corrections, military, and other personnel involved in emergency response operations, the protection against blunt impact threats can be a matter of life or death. To quantify the levels of protection of a Blunt Trauma PPE, users and industry rely on technical standards. A balance between protection and functionality allow users to have good flexibility and mobility. Good air ventilation underneath the PPE suit can protect users against heat stroke or hyperthermia.
The Pediatric Risk of Mortality (PRISM) score was developed from the Physiologic Stability Index (PSI) to reduce the number of physiologic variables required for pediatric intensive-care unit (PICU) mortality risk assessment, from 34 to 14, and to obtain an objective weighting of the remaining variables.

Trauma in children, also known as pediatric trauma, refers to a traumatic injury that happens to an infant, child or adolescent. Because of anatomical and physiological differences between children and adults the care and management of this population differs.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50 mmHg or systolic blood pressure of less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury, some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding are thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
Fraction of inspired oxygen (FIO2), correctly denoted with a capital I, is the molar or volumetric fraction of oxygen in the inhaled gas. Medical patients experiencing difficulty breathing are provided with oxygen-enriched air, which means a higher-than-atmospheric FIO2. Natural air includes 21% oxygen, which is equivalent to FIO2 of 0.21. Oxygen-enriched air has a higher FIO2 than 0.21; up to 1.00 which means 100% oxygen. FIO2 is typically maintained below 0.5 even with mechanical ventilation, to avoid oxygen toxicity, but there are applications when up to 100% is routinely used.