Cardiac tamponade, also known as pericardial tamponade, is a compression of the heart due to pericardial effusion. Onset may be rapid or gradual. Symptoms typically include those of obstructive shock including shortness of breath, weakness, lightheadedness, and cough. Other symptoms may relate to the underlying cause.
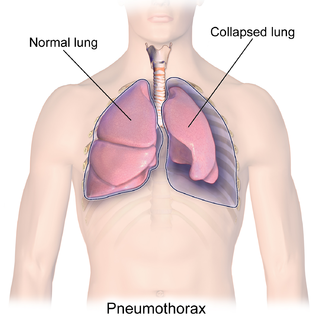
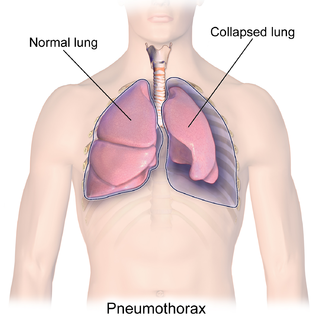
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed by an area of damaged tissue, and the amount of air in the space between chest wall and lungs increases; this is called a tension pneumothorax. This can cause a steadily worsening oxygen shortage and low blood pressure. This leads to a type of shock called obstructive shock, which can be fatal unless reversed. Very rarely, both lungs may be affected by a pneumothorax. It is often called a "collapsed lung", although that term may also refer to atelectasis.

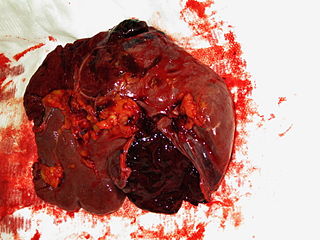
Internal bleeding is a loss of blood from a blood vessel that collects inside the body. Internal bleeding is usually not visible from the outside. It is a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding. Severe internal bleeding into the chest, abdomen, retroperitoneal space, pelvis, and thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly. Internal bleeding is a medical emergency and should be treated immediately by medical professionals.

A chest tube is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum in order to remove clinically undesired substances such as air (pneumothorax), excess fluid, blood (hemothorax), chyle (chylothorax) or pus (empyema) from the intrathoracic space. An intrapleural chest tube is also known as a Bülau drain or an intercostal catheter (ICC), and can either be a thin, flexible silicone tube, or a larger, semi-rigid, fenestrated plastic tube, which often involves a flutter valve or underwater seal.

Traumatic cardiac arrest (TCA) is a condition in which the heart has ceased to beat due to blunt or penetrating trauma, such as a stab wound to the thoracic area. It is a medical emergency which will always result in death without prompt advanced medical care. Even with prompt medical intervention, survival without neurological complications is rare. In recent years, protocols have been proposed to improve survival rate in patients with traumatic cardiac arrest, though the variable causes of this condition as well as many coexisting injuries can make these protocols difficult to standardize. Traumatic cardiac arrest is a complex form of cardiac arrest often derailing from advanced cardiac life support in the sense that the emergency team must first establish the cause of the traumatic arrest and reverse these effects, for example hypovolemia and haemorrhagic shock due to a penetrating injury.

The mediastinum is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is an undelineated region that contains a group of structures within the thorax, namely the heart and its vessels, the esophagus, the trachea, the phrenic and cardiac nerves, the thoracic duct, the thymus and the lymph nodes of the central chest.

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to Pneumothorax, or rarely in association with other conditions.
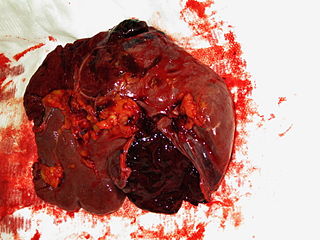
A splenic injury, which includes a ruptured spleen, is any injury to the spleen. The rupture of a normal spleen can be caused by trauma, such as a traffic collision.

A pericardial effusion is an abnormal accumulation of fluid in the pericardial cavity. The pericardium is a two-part membrane surrounding the heart: the outer fibrous connective membrane and an inner two-layered serous membrane. The two layers of the serous membrane enclose the pericardial cavity between them. This pericardial space contains a small amount of pericardial fluid. The fluid is normally 15-50 mL in volume. The pericardium, specifically the pericardial fluid provides lubrication, maintains the anatomic position of the heart in the chest, and also serves as a barrier to protect the heart from infection and inflammation in adjacent tissues and organs.

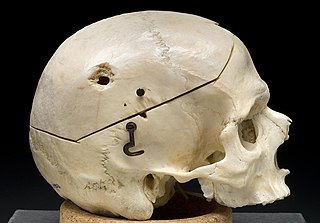
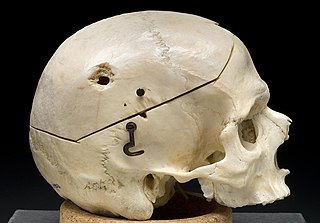
Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma occurs frequently where there is direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, direct physical blows, assaults, sports-related injuries, and are notably common among the elderly who experience falls. Blunt trauma injuries can be categorized into four primary types: contusions (bruise), abrasions, lacerations, and fractures. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound.

A chest injury, also known as chest trauma, is any form of physical injury to the chest including the ribs, heart and lungs. Chest injuries account for 25% of all deaths from traumatic injury. Typically chest injuries are caused by blunt mechanisms such as direct, indirect, compression, contusion, deceleration, or blasts caused by motor vehicle collisions or penetrating mechanisms such as stabbings.

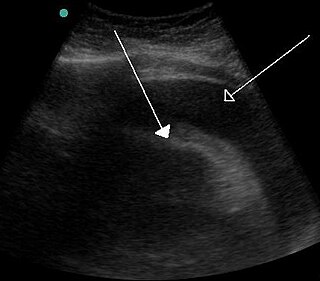
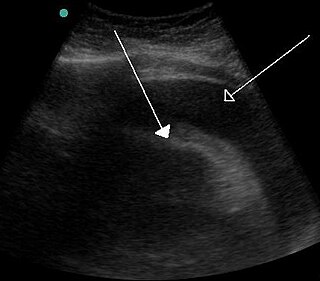
Focused assessment with sonography in trauma is a rapid bedside ultrasound examination performed by surgeons, emergency physicians, and paramedics as a screening test for blood around the heart or abdominal organs (hemoperitoneum) after trauma. There is also the extended FAST (eFAST) which includes some additional ultrasound views to assess for pneumothorax.
A gunshot wound (GSW) is a penetrating injury caused by a projectile from a gun. Damages may include bleeding, bone fractures, organ damage, wound infection, loss of the ability to move part of the body, and in severe cases, death. Damage depends on the part of the body hit, the path the bullet follows through the body, and the type and speed of the bullet. Long-term complications can include bowel obstruction, failure to thrive, neurogenic bladder and paralysis, recurrent cardiorespiratory distress and pneumothorax, hypoxic brain injury leading to early dementia, amputations, chronic pain and pain with light touch (hyperalgesia), deep venous thrombosis with pulmonary embolus, limb swelling and debility, and lead poisoning.
Lung cancer staging is the assessment of the extent to which a lung cancer has spread from its original source. As with most cancers, staging is an important determinant of treatment and prognosis. In general, more advanced stages of cancer are less amenable to treatment and have a worse prognosis.

A pulmonary laceration is a chest injury in which lung tissue is torn or cut. An injury that is potentially more serious than pulmonary contusion, pulmonary laceration involves disruption of the architecture of the lung, while pulmonary contusion does not. Pulmonary laceration is commonly caused by penetrating trauma but may also result from forces involved in blunt trauma such as shear stress. A cavity filled with blood, air, or both can form. The injury is diagnosed when collections of air or fluid are found on a CT scan of the chest. Surgery may be required to stitch the laceration, to drain blood, or even to remove injured parts of the lung. The injury commonly heals quickly with few problems if it is given proper treatment; however it may be associated with scarring of the lung or other complications.

Subcutaneous emphysema occurs when gas or air accumulates and seeps under the skin, where normally no gas should be present. Subcutaneous refers to the subcutaneous tissue, and emphysema refers to trapped air pockets. Since the air generally comes from the chest cavity, subcutaneous emphysema usually occurs around the upper torso, such as on the chest, neck, face, axillae and arms, where it is able to travel with little resistance along the loose connective tissue within the superficial fascia. Subcutaneous emphysema has a characteristic crackling-feel to the touch, a sensation that has been described as similar to touching warm Rice Krispies. This sensation of air under the skin is known as subcutaneous crepitation, a form of crepitus.

Abdominal trauma is an injury to the abdomen. Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Complications may include blood loss and infection.

Diaphragmatic rupture is a tear of the diaphragm, the muscle across the bottom of the ribcage that plays a crucial role in breathing. Most commonly, acquired diaphragmatic tears result from physical trauma. Diaphragmatic rupture can result from blunt or penetrating trauma and occurs in about 0.5% of all people with trauma.

Injury of the thoracic aorta refers to any injury which affects the portion of the aorta which lies within the chest cavity. Injuries of the thoracic aorta are usually the result of physical trauma; however, they can also be the result of a pathological process. The main causes of this injury are deceleration and crush injuries. There are different grades to injuries to the aorta depending on the extent of injury, and the treatment whether surgical or medical depends on that grade. It is difficult to determine if a patient has a thoracic injury just by their symptoms, but through imaging and a physical exam the extent of injury can be determined. All patients with a thoracic aortic injury need to be treated either surgically with endovascular repair or open surgical repair or with medicine to keep their blood pressure and heart rate in the appropriate range. However, most patients that have a thoracic aortic injury do not live for 24 hours.

A resuscitative thoracotomy (sometimes referred to as an emergency department thoracotomy (EDT), trauma thoracotomy or, colloquially, as "cracking the chest") is a thoracotomy performed to resuscitate a major trauma patient who has sustained severe thoracic or abdominal trauma and who has entered cardiac arrest because of this. The procedure allows immediate direct access to the thoracic cavity, permitting rescuers to control hemorrhage, relieve cardiac tamponade, repair or control major injuries to the heart, lungs or thoracic vasculature, and perform direct cardiac massage or defibrillation. The procedure is rarely performed and is a procedure of last resort.