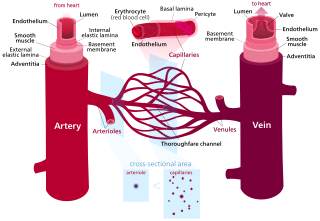
An artery is a blood vessel in humans and most other animals that takes oxygenated blood away from the heart in the systemic circulation to one or more parts of the body. Exceptions that carry deoxygenated blood are the pulmonary arteries in the pulmonary circulation that carry blood to the lungs for oxygenation, and the umbilical arteries in the fetal circulation that carry deoxygenated blood to the placenta. It consists of a multi-layered artery wall wrapped into a tube-shaped channel.
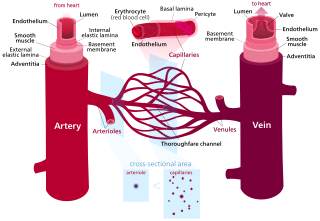
Blood vessels are the structures of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from the tissues. Blood vessels are needed to sustain life, because all of the body's tissues rely on their functionality.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

A capillary is a small blood vessel, from 5 to 10 micrometres in diameter, and is part of the microcirculation system. Capillaries are microvessels and the smallest blood vessels in the body. They are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the site of the exchange of many substances from the surrounding interstitial fluid, and they convey blood from the smallest branches of the arteries (arterioles) to those of the veins (venules). Other substances which cross capillaries include water, oxygen, carbon dioxide, urea, glucose, uric acid, lactic acid and creatinine. Lymph capillaries connect with larger lymph vessels to drain lymphatic fluid collected in microcirculation.
Hemodynamics or haemodynamics are the dynamics of blood flow. The circulatory system is controlled by homeostatic mechanisms of autoregulation, just as hydraulic circuits are controlled by control systems. The hemodynamic response continuously monitors and adjusts to conditions in the body and its environment. Hemodynamics explains the physical laws that govern the flow of blood in the blood vessels.

Smooth (soft) muscle is one of the three major types of vertebrate muscle tissue, the other being skeletal and cardiac muscle. Nonetheless, it is found in invertebrates as well and is controlled by the autonomic nervous system. It is non-striated, so-called because it has no sarcomeres and therefore no striations. It can be divided into two subgroups, single-unit and multi-unit smooth muscle. Within single-unit muscle, the whole bundle or sheet of smooth muscle cells contracts as a syncytium.

The microcirculation is the circulation of the blood in the smallest blood vessels, the microvessels of the microvasculature present within organ tissues. The microvessels include terminal arterioles, metarterioles, capillaries, and venules. Arterioles carry oxygenated blood to the capillaries, and blood flows out of the capillaries through venules into veins.

Vasodilation, also known as vasorelaxation, is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. Blood vessel walls are composed of endothelial tissue and a basal membrane lining the lumen of the vessel, concentric smooth muscle layers on top of endothelial tissue, and an adventitia over the smooth muscle layers. Relaxation of the smooth muscle layer allows the blood vessel to dilate, as it is held in a semi-constricted state by sympathetic nervous system activity. Vasodilation is the opposite of vasoconstriction, which is the narrowing of blood vessels.

A venule is a very small vein in the microcirculation that allows blood to return from the capillary beds to drain into the venous system via increasingly larger veins. Post-capillary venules are the smallest of the veins with a diameter of between 10 and 30 micrometres (μm). When the post-capillary venules increase in diameter to 50μm they can incorporate smooth muscle and are known as muscular venules. Veins contain approximately 70% of total blood volume, while about 25% is contained in the venules. Many venules unite to form a vein.
Vascular resistance is the resistance that must be overcome for blood to flow through the circulatory system. The resistance offered by the systemic circulation is known as the systemic vascular resistance (SVR) or may sometimes be called by the older term total peripheral resistance (TPR), while the resistance offered by the pulmonary circulation is known as the pulmonary vascular resistance (PVR). Systemic vascular resistance is used in calculations of blood pressure, blood flow, and cardiac function. Vasoconstriction increases SVR, whereas vasodilation decreases SVR.

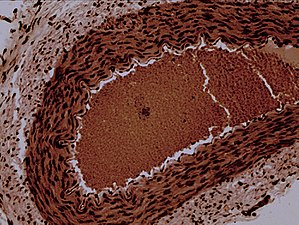
In the kidney, the macula densa is an area of closely packed specialized cells lining the wall of the distal tubule where it touches the glomerulus. Specifically, the macula densa is found in the terminal portion of the distal straight tubule, after which the distal convoluted tubule begins.
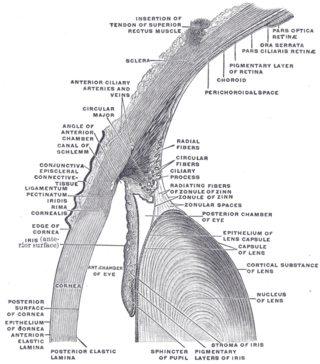
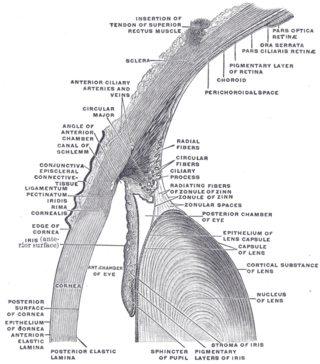
In the anatomy of the eye, the conjunctiva is a thin mucous membrane that lines the inside of the eyelids and covers the sclera. It is composed of non-keratinized, stratified squamous epithelium with goblet cells, stratified columnar epithelium and stratified cuboidal epithelium. The conjunctiva is highly vascularised, with many microvessels easily accessible for imaging studies.

An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm.
Hyperaemia is the increase of blood flow to different tissues in the body. It can have medical implications but is also a regulatory response, allowing change in blood supply to different tissues through vasodilation. Clinically, hyperaemia in tissues manifests as erythema because of the engorgement of vessels with oxygenated blood. Hyperaemia can also occur due to a fall in atmospheric pressure outside the body. The term comes from Greek ὑπέρ (hupér) 'over', and αἷμα (haîma) 'blood'.
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. It is one of four categories of shock, a condition where there is not enough oxygen-carrying blood to meet the metabolic needs of the cells which make up the body's tissues and organs. Distributive shock is different from the other three categories of shock in that it occurs even though the output of the heart is at or above a normal level. The most common cause is sepsis leading to a type of distributive shock called septic shock, a condition that can be fatal.

Arteriolosclerosis is a form of cardiovascular disease involving hardening and loss of elasticity of arterioles or small arteries and is most often associated with hypertension and diabetes mellitus. Types include hyaline arteriolosclerosis and hyperplastic arteriolosclerosis, both involved with vessel wall thickening and luminal narrowing that may cause downstream ischemic injury. The following two terms whilst similar, are distinct in both spelling and meaning and may easily be confused with arteriolosclerosis.
The myogenic mechanism is how arteries and arterioles react to an increase or decrease of blood pressure to keep the blood flow constant within the blood vessel. Myogenic response refers to a contraction initiated by the myocyte itself instead of an outside occurrence or stimulus such as nerve innervation. Most often observed in smaller resistance arteries, this 'basal' myogenic tone may be useful in the regulation of organ blood flow and peripheral resistance, as it positions a vessel in a preconstricted state that allows other factors to induce additional constriction or dilation to increase or decrease blood flow.
Microvasculature comprises the microvessels – venules and capillaries of the microcirculation, with a maximum average diameter of 0.3 millimeters. As the vessels decrease in size, they increase their surface-area-to-volume ratio. This allows surface properties to play a significant role in the function of the vessel.
In physiology, acute local blood flow regulation refers to an intrinsic regulation, or control, of the vascular tone of arteries at a local level, meaning within a certain tissue type, organ, or organ system. This intrinsic type of control means that the blood vessels can automatically adjust their own vascular tone, by dilating (widening) or constricting (narrowing), in response to some change in the environment. This change occurs in order to match up the tissue's oxygen demand with the actual oxygen supply available in the blood as closely as possible. For example, if a muscle is being utilized actively, it will require more oxygen than it was at rest, so the blood vessels supplying that muscle will vasodilate, or widen in size, to increase the amount of blood, and therefore oxygen, being delivered to that muscle.
A resistance artery is small diameter blood vessel in the microcirculation that contributes significantly to the creation of the resistance to flow and regulation of blood flow. Resistance arteries are usually small arteries or arterioles and include precapillary sphincters. Having thick muscular walls and narrow lumen they contribute the most to the resistance to blood flow. Degree of the contraction of vascular smooth muscle in the wall of a resistance artery is directly connected to the size of the lumen.