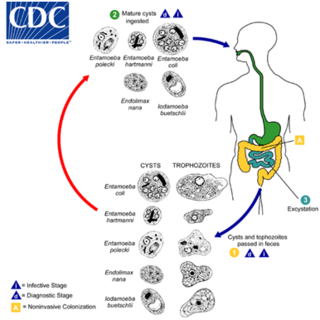
Entamoeba is a genus of Amoebozoa found as internal parasites or commensals of animals. In 1875, Fedor Lösch described the first proven case of amoebic dysentery in St. Petersburg, Russia. He referred to the amoeba he observed microscopically as Amoeba coli; however, it is not clear whether he was using this as a descriptive term or intended it as a formal taxonomic name. The genus Entamoeba was defined by Casagrandi and Barbagallo for the species Entamoeba coli, which is known to be a commensal organism. Lösch's organism was renamed Entamoeba histolytica by Fritz Schaudinn in 1903; he later died, in 1906, from a self-inflicted infection when studying this amoeba. For a time during the first half of the 20th century the entire genus Entamoeba was transferred to Endamoeba, a genus of amoebas infecting invertebrates about which little is known. This move was reversed by the International Commission on Zoological Nomenclature in the late 1950s, and Entamoeba has stayed 'stable' ever since.
Diarrhea, also spelled diarrhoea or diarrhœa, is the condition of having at least three loose, liquid, or watery bowel movements in a day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin with loss of the normal stretchiness of the skin and irritable behaviour. This can progress to decreased urination, loss of skin color, a fast heart rate, and a decrease in responsiveness as it becomes more severe. Loose but non-watery stools in babies who are exclusively breastfed, however, are normal.

Shigellosis, known historically as dysentery, is an infection of the intestines caused by Shigella bacteria. Symptoms generally start one to two days after exposure and include diarrhea, fever, abdominal pain, and feeling the need to pass stools even when the bowels are empty. The diarrhea may be bloody. Symptoms typically last five to seven days and it may take several months before bowel habits return entirely to normal. Complications can include reactive arthritis, sepsis, seizures, and hemolytic uremic syndrome.

Shigella is a genus of bacteria that is Gram negative, facultatively anaerobic, non–spore-forming, nonmotile, rod shaped, and is genetically nested within Escherichia. The genus is named after Kiyoshi Shiga, who discovered it in 1897.

Entamoeba histolytica is an anaerobic parasitic amoebozoan, part of the genus Entamoeba. Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated to infect about 35-50 million people worldwide. E. histolytica infection is estimated to kill more than 55,000 people each year. Previously, it was thought that 10% of the world population was infected, but these figures predate the recognition that at least 90% of these infections were due to a second species, E. dispar. Mammals such as dogs and cats can become infected transiently, but are not thought to contribute significantly to transmission.

The fecal–oral route describes a particular route of transmission of a disease wherein pathogens in fecal particles pass from one person to the mouth of another person. Main causes of fecal–oral disease transmission include lack of adequate sanitation, and poor hygiene practices. If soil or water bodies are polluted with fecal material, humans can be infected with waterborne diseases or soil-transmitted diseases. Fecal contamination of food is another form of fecal-oral transmission. Washing hands properly after changing a baby's diaper or after performing anal hygiene can prevent foodborne illness from spreading.
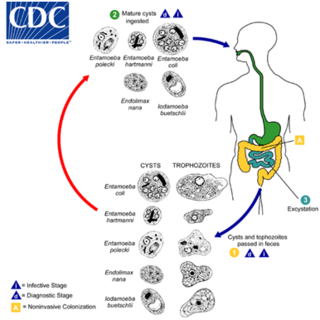
Entamoeba coli is a non-pathogenic species of Entamoeba that frequently exists as a commensal parasite in the human gastrointestinal tract. E. coli is important in medicine because it can be confused during microscopic examination of stained stool specimens with the pathogenic Entamoeba histolytica. While this differentiation is typically done by visual examination of the parasitic cysts via light microscopy, new methods using molecular biology techniques have been developed.

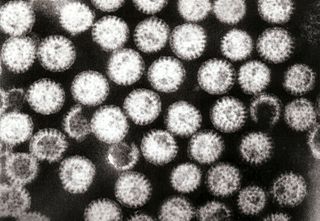
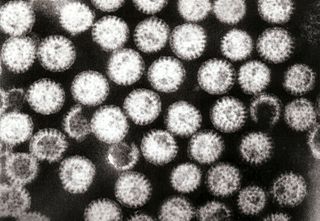
Amoebozoa is a major taxonomic group containing about 2,400 described species of amoeboid protists, often possessing blunt, fingerlike, lobose pseudopods and tubular mitochondrial cristae. In traditional classification schemes, Amoebozoa is usually ranked as a phylum within either the kingdom Protista or the kingdom Protozoa. In the classification favored by the International Society of Protistologists, it is retained as an unranked "supergroup" within Eukaryota. Molecular genetic analysis supports Amoebozoa as a monophyletic clade. Modern studies of eukaryotic phylogenetic trees identify it as the sister group to Opisthokonta, another major clade which contains both fungi and animals as well as several other clades comprising some 300 species of unicellular eukaryotes. Amoebozoa and Opisthokonta are sometimes grouped together in a high-level taxon, named Amorphea. Amoebozoa includes many of the best-known amoeboid organisms, such as Chaos, Entamoeba, Pelomyxa and the genus Amoeba itself. Species of Amoebozoa may be either shelled (testate) or naked, and cells may possess flagella. Free-living species are common in both salt and freshwater as well as soil, moss and leaf litter. Some live as parasites or symbionts of other organisms, and some are known to cause disease in humans and other organisms.

Gastroenteritis, also known as infectious diarrhea, is an inflammation of the gastrointestinal tract including the stomach and intestine. Symptoms may include diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. This typically lasts less than two weeks. Although it is not related to influenza, in the U.S. and U.K., it is sometimes called the "stomach flu".
Endolimax is a genus of amoebozoa that are found in the intestines of various animals, including the species E. nana found in humans. Originally thought to be non-pathogenic, studies suggest it can cause intermittent or chronic diarrhea. Additionally, it is very significant in medicine because it can provide false positives for other tests, notably the similar species Entamoeba histolytica, the pathogen responsible for amoebic dysentery, and because its presence indicates the host has consumed fecal material. It forms cysts with four nuclei which excyst in the body and become trophozoites. Endolimax nana nuclei have a large endosome somewhat off-center and small amounts of visible chromatin or none at all.
Bacillary dysentery is a type of dysentery, and is a severe form of shigellosis. It is associated with species of bacteria from the family Enterobacteriaceae. The term is usually restricted to Shigella infections.
Enterocolitis is an inflammation of the digestive tract, involving enteritis of the small intestine and colitis of the colon. It may be caused by various infections, with bacteria, viruses, fungi, parasites, or other causes. Common clinical manifestations of enterocolitis are frequent diarrheal defecations, with or without nausea, vomiting, abdominal pain, fever, chills, and alteration of general condition. General manifestations are given by the dissemination of the infectious agent or its toxins throughout the body, or – most frequently – by significant losses of water and minerals, the consequence of diarrhea and vomiting.
Dientamoebiasis is a medical condition caused by infection with Dientamoeba fragilis, a single-cell parasite that infects the lower gastrointestinal tract of humans. It is an important cause of traveler's diarrhea, chronic abdominal pain, chronic fatigue, and failure to thrive in children.

Protozoan infections are parasitic diseases caused by organisms formerly classified in the kingdom Protozoa. These organisms are now classified in the supergroups Excavata, Amoebozoa, Harosa, and Archaeplastida. They are usually contracted by either an insect vector or by contact with an infected substance or surface.

Shigella sonnei is a species of Shigella. Together with Shigella flexneri, it is responsible for 90% of shigellosis cases. Shigella sonnei is named for the Danish bacteriologist Carl Olaf Sonne. It is a Gram-negative, rod-shaped, nonmotile, non-spore-forming bacterium.

Amoebiasis, or amoebic dysentery, is an infection of the intestines caused by a parasitic amoeba Entamoeba histolytica. Amoebiasis can be present with no, mild, or severe symptoms. Symptoms may include lethargy, loss of weight, colonic ulcerations, abdominal pain, diarrhea, or bloody diarrhea. Complications can include inflammation and ulceration of the colon with tissue death or perforation, which may result in peritonitis. Anemia may develop due to prolonged gastric bleeding.

A amoebic liver abscess is a type of liver abscess caused by amebiasis. It is the involvement of liver tissue by trophozoites of the organism Entamoeba histolytica and of its abscess due to necrosis.

Amoebic brain abscess is an affliction caused by the anaerobic parasitic protist Entamoeba histolytica. It is extremely rare; the first case being reported in 1849. Brain abscesses resulting from Entamoeba histolytica are difficult to diagnose and very few case reports suggest complete recovery even after the administration of appropriate treatment regimen.
Enteroinvasive Escherichia coli (EIEC) is a type of pathogenic bacteria whose infection causes a syndrome that is identical to shigellosis, with profuse diarrhea and high fever. EIEC are highly invasive, and they use adhesin proteins to bind to and enter intestinal cells. They produce no toxins, but severely damage the intestinal wall through mechanical cell destruction.
Entamoeba moshkovskii is part of the genus Entamoeba. It is found in areas with polluted water sources, and is prevalent in places such as Malaysia, India, and Bangladesh, but more recently has made its way to Turkey, Australia, and North America. This amoeba is said to rarely infect humans, but recently this has changed. It is in question as to whether it is pathogenic or not. Despite some sources stating this is a free living amoeba, various studies worldwide have shown it contains the ability to infect humans, with some cases of pathogenic potential being reported. Some of the symptoms that often occur are diarrhea, weight loss, bloody stool, and abdominal pain. The first known human infection also known as the "Laredo strain" of Entamoebic mushkovskii was in Laredo, Texas in 1991, although it was first described by a man named Tshalaia in 1941 in Moscow, Russia. It is known to affect people of all ages and genders.