| Tularemia | |
|---|---|
| Other names | Tularaemia, Pahvant Valley plague, [1] rabbit fever, [1] deer fly fever, Ohara's fever [2] |
 | |
| A tularemia lesion on the back of the right hand | |
| Specialty | Infectious disease |
| Symptoms | Fever, skin ulcer, large lymph nodes [3] |
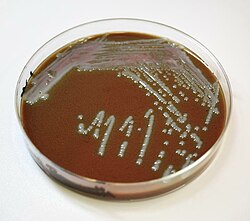
| Causes | bacterium Francisella tularensis (spread by ticks, deer flies, contact with infected animals) [4] |
| Diagnostic method | Blood tests, microbial culture [5] |
| Prevention | Insect repellent, wearing long pants, rapidly removing ticks, not disturbing dead animals [6] |
| Medication | Aminoglycosides (Streptomycin, Gentamicin), doxycycline, ciprofloxacin [5] |
| Prognosis | Generally good with treatment [4] |
| Frequency | ~200 cases per year (US) [7] |
Tularemia, also known as rabbit fever, is an infectious disease caused by the bacterium Francisella tularensis . [4] Symptoms may include fever, skin ulcers, and enlarged lymph nodes. [3] Occasionally, a form that results in pneumonia or a throat and nasal sinus infection may occur. [3]
Contents
- Signs and symptoms
- Cause
- Bacteria
- Spread
- Diagnosis
- Pathology
- Prevention
- Treatment
- Prognosis
- Epidemiology
- Outbreaks
- History
- Use as a biological weapon
- Other animals
- References
The bacterium is typically spread by ticks, deer flies, or contact with infected animals. [4] It may also be spread by drinking contaminated water or breathing in contaminated dust. [4] It does not spread directly between people. [8] Diagnosis is by blood tests or cultures of the infected site. [5] [9]
Prevention includes the use of insect repellent and long pants, rapidly removing ticks, and not disturbing dead animals. [6] Treatment is typically with the antibiotic streptomycin. [9] Gentamicin, doxycycline, or ciprofloxacin may also be used. [5]
Between the 1970s and 2015, around 200 cases were reported in the United States each year. [7] Males are affected more often than females. [7] It occurs most frequently in the young and the middle-aged. [7] In the United States, most cases occur in the summer. [7] The disease is named after Tulare County, California, where the disease was discovered in 1911. [10] Several other animals, such as rabbits, may also be infected. [4]