| Pyomyositis | |
|---|---|
| Other names | Tropical pyomyositis or Myositis tropicans |
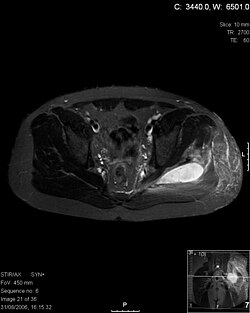 | |
| Transverse T2 magnetic resonance imaging section through the hip region showing abscess collection in a patient with pyomyositis. | |
| Specialty | Rheumatology |
| Diagnostic method | Diagnostic method used for PM includes ultrasound, CT scan and MRI. Ultrasound can be helpful in showing muscular heterogeneity or a purulent collection but it is not useful during the first stage of the disease. CT scan can confirm the diagnosis before abscesses occur with enlargement of the involved muscles and hypodensity when abscess is present, terogenous attenuation and fluid collection with rim enhancement can be found. MRI is useful to assess PM and determine its localization and extension |
Pyomyositis (Myositis tropicans) is a bacterial infection of the skeletal muscles which results in an abscess. Pyomyositis is most common in tropical areas but can also occur in temperate zones.
Contents
Pyomyositis can be classified as primary or secondary. Primary pyomyositis is a skeletal muscle infection arising from hematogenous infection, whereas secondary pyomyositis arises from localized penetrating trauma or contiguous spread to the muscle. [1]




