| Oral rehydration therapy | |
|---|---|
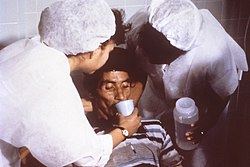
 An oral rehydration solution (250ml) prepared according to WHO formula. | |
| Other names | oral rehydration solution (ORS), oral rehydration salts (ORS), glucose-salt solution |
Oral rehydration therapy (ORT) is a type of fluid replacement used to prevent and treat dehydration, especially due to diarrhea. [1] It involves drinking water with modest amounts of sugar and salts, specifically sodium and potassium. [1] Oral rehydration therapy can also be given by a nasogastric tube. [1] Therapy can include the use of zinc supplements to reduce the duration of diarrhea in infants and children under the age of 5. [1] Use of oral rehydration therapy has been estimated to decrease the risk of death from diarrhea by up to 93%. [2]
Contents
- Medical uses
- Efficacy
- Treatment algorithm
- Contraindications
- Preparation
- Reduced-osmolarity
- Administration
- Associated therapies
- Zinc
- Feeding
- Children with malnutrition
- Antibiotics
- Physiological basis
- History
- Definition
- Development
- Awards
- References
- Further reading
- External links
Side effects may include vomiting, high blood sodium, or high blood potassium. [1] If vomiting occurs, it is recommended that use be paused for 10 minutes and then gradually restarted. [1] The recommended formulation includes sodium chloride, sodium citrate, potassium chloride, and glucose. [1] Glucose may be replaced by sucrose and sodium citrate may be replaced by sodium bicarbonate, if not available, although the resulting mixture is not shelf stable in high-humidity environments. [1] [3] It works as glucose increases the uptake of sodium and thus water by the intestines, and the potassium chloride and sodium citrate help prevent hypokalemia and acidosis, respectively, which are both common side effects of diarrhea. [4] [3] [5] A number of other formulations are also available including versions that can be made at home. [4] [2] However, the use of homemade solutions has not been well studied. [2]
Oral rehydration therapy was developed in the 1940s using electrolyte solutions with or without glucose on an empirical basis chiefly for mild or convalescent patients, but did not come into common use for rehydration and maintenance therapy until after the discovery that glucose promoted sodium and water absorption during cholera in the 1960s. [6] It is on the World Health Organization's List of Essential Medicines. [7] Globally, as of 2015 [update] , oral rehydration therapy is used by 41% of children with diarrhea. [8] This use has played an important role in reducing the number of deaths in children under the age of five. [8]