| Foreign body granuloma | |
|---|---|
 | |
| Transvaginal ultrasonography showing a foreign body granuloma at right as a hypoechoic (dark) area around a perforated intrauterine device. The uterus is at left. | |
| Specialty | Dermatology |
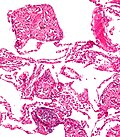
A foreign body reaction (FBR) is a typical tissue response to a foreign body within biological tissue. [1] It usually includes the formation of a foreign body granuloma . [2] Tissue encapsulation of an implant is an example, as is inflammation around a splinter. [3] Foreign body granuloma formation consists of protein adsorption, macrophages, multinucleated foreign body giant cells (macrophage fusion), fibroblasts, and angiogenesis. It has also been proposed that the mechanical property of the interface between an implant and its surrounding tissues is critical for the host response. [4] [5]
Contents
- Foreign body reaction to biomaterial implantation
- Protein adsorption
- Immune recruitment
- Macrophage fusion
- Fibrous capsule formation
- Engineering biomaterial to resist the foreign body reaction
- Modification of physical properties
- Delivery of anti-inflammatory drugs
- Incorporation of bioactive molecules
- Novel biomaterials
- Gallery
- See also
- References
- External links
In the long term, the foreign body reaction results in encapsulation of the foreign body within a calcified shell. For example, a lithopedion is a rare phenomenon which occurs most commonly when a fetus dies during an abdominal pregnancy, [6] is too large to be reabsorbed by the body, and calcifies.