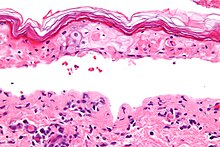
Stevens–Johnson syndrome (SJS) is a type of severe skin reaction. Together with toxic epidermal necrolysis (TEN) and Stevens–Johnson/toxic epidermal necrolysis (SJS/TEN) overlap, they are considered febrile mucocutaneous drug reactions and probably part of the same spectrum of disease, with SJS being less severe. Erythema multiforme (EM) is generally considered a separate condition. Early symptoms of SJS include fever and flu-like symptoms. A few days later, the skin begins to blister and peel, forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia and multiple organ failure.

Toxic epidermal necrolysis (TEN), also known as Lyell's syndrome, is a type of severe skin reaction. Together with Stevens–Johnson syndrome (SJS) it forms a spectrum of disease, with TEN being more severe. Early symptoms include fever and flu-like symptoms. A few days later the skin begins to blister and peel forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia, and multiple organ failure.

Erythema multiforme (EM) is a skin condition that appears with red patches evolving into target lesions, typically on both hands.

Staphylococcal scalded skin syndrome (SSSS) is a dermatological condition caused by Staphylococcus aureus.

Tetrazepam is a benzodiazepine derivative with anticonvulsant, anxiolytic, muscle relaxant and slightly hypnotic properties. It was formerly used mainly in Austria, France, Belgium, Germany and Spain to treat muscle spasm, anxiety disorders such as panic attacks, or more rarely to treat depression, premenstrual syndrome or agoraphobia. Tetrazepam has relatively little sedative effect at low doses while still producing useful muscle relaxation and anxiety relief. The Co-ordination Group for Mutual Recognition and Decentralised Procedures-Human endorsed the Pharmacovigilance Risk Assessment Committee (PRAC) recommendation to suspend the marketing authorisations of tetrazepam-containing medicines across the European Union (EU) in April 2013. The European Commission has confirmed the suspension of the marketing authorisations for Tetrazepam in Europe because of cutaneous toxicity, effective from the 1 August 2013.

Tenoxicam, sold under the brand name Mobiflex among others, is a nonsteroidal anti-inflammatory drug (NSAID). It is used to relieve inflammation, swelling, stiffness, and pain associated with rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, tendinitis, bursitis, and periarthritis of the shoulders or hips.

Oxicam is a class of non-steroidal anti-inflammatory drugs (NSAIDs), meaning that they have anti-inflammatory, analgesic, and antipyretic therapeutic effects. Oxicams bind closely to plasma proteins. Most oxicams are unselective inhibitors of the cyclooxygenase (COX) enzymes. The exception is meloxicam with a slight (10:1) preference for COX-2, which, however, is only clinically relevant at low doses.
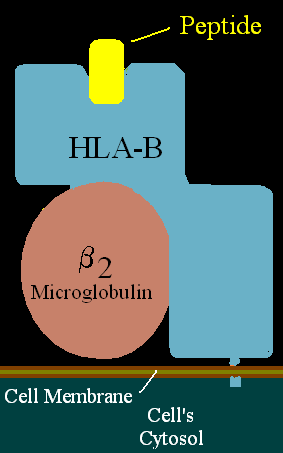
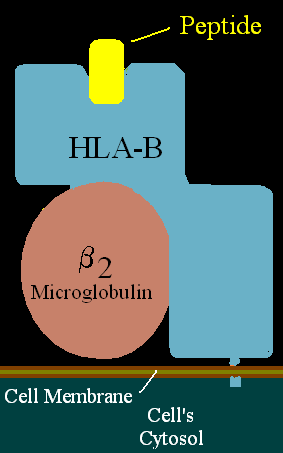
HLA-B58 (B58) is an HLA-B serotype. B58 is a split antigen from the B17 broad antigen, the sister serotype B57. The serotype identifies the more common HLA-B*58 gene products. B*5801 is associated with allopurinol induced inflammatory necrotic skin disease.

In medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.
Paraneoplastic pemphigus (PNP) is an autoimmune disorder stemming from an underlying tumor. It is hypothesized that antigens associated with the tumor trigger an immune response resulting in blistering of the skin and mucous membranes.
Anticonvulsant/sulfonamide hypersensitivity syndrome is a potentially serious hypersensitivity reaction that can be seen with medications with an aromatic amine chemical structure, such as aromatic anticonvulsants, sulfonamides, or other medications with an aromatic amine. Cross-reactivity should not occur between medications with an aromatic amine and medications without an aromatic amine ; therefore, these medications can be safely used in the future.

Allopurinol hypersensitivity syndrome(AHS) typically occurs in persons with preexisting kidney failure. Weeks to months after allopurinol is begun, the patient develops a morbilliform eruption or, less commonly, develops one of the far more serious and potentially lethal severe cutaneous adverse reactions viz., the DRESS syndrome, Stevens Johnson syndrome, or toxic epidermal necrolysis. About 1 in 1000 patients receiving allopurinol are affected, and mortality rates have been reported to be between 20% and 25%.

Acute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication.

Generalized bullous fixed drug eruption (GBFDE) most commonly refers to a drug reaction in the erythema multiforme group. These are uncommon reactions to medications, with an incidence of 0.4 to 1.2 per million person-years for toxic epidermal necrolysis and 1.2 to 6.0 per million person-years for Stevens–Johnson syndrome. The primary skin lesions are large erythemas, most often irregularly distributed and of a characteristic purplish-livid color, at times with flaccid blisters.

Abacavir/dolutegravir/lamivudine, sold under the brand name Triumeq among others, is a fixed-dose combination antiretroviral medication for the treatment of HIV/AIDS. It is a combination of three medications with different and complementary mechanisms of action: abacavir, dolutegravir and lamivudine.
Severe cutaneous adverse reactions are a group of potentially lethal adverse drug reactions that involve the skin and mucous membranes of various body openings such as the eyes, ears, and inside the nose, mouth, and lips. In more severe cases, SCARs also involves serious damage to internal organs. SCARs includes five syndromes: Drug reaction with eosinophilia and systemic symptoms ; Stevens–Johnson syndrome (SJS); Toxic epidermal necrolysis (TEN), Stevens-Johnson/toxic epidermal necrolysis overlap syndrome (SJS/TEN); and Acute generalized exanthematous pustulosis (AGEP). The five disorders have similar pathophysiologies, i.e. disease-causing mechanisms, for which new strategies are in use or development to identify individuals predisposed to develop the SCARs-inducing effects of specific drugs and thereby avoid treatment with them. Maculopapular rash (MPR) is a less-well defined and benign form of drug-induced adverse skin reactions; while not classified in the SCARs group, it shares a similar pathophysiology with SCARs and is caused by some of the same drugs which cause SCARs.
The p-i concept refers to the pharmacological interaction of drugs with immune receptors. It explains a form of drug hypersensitivity, namely T cell stimulation, which can lead to various acute inflammatory manifestations such as exanthems, eosinophilia and systemic symptoms, Stevens–Johnson syndrome, toxic epidermal nercrolysis, and complications upon withdrawing the drug.
5. Orphanet Journal of Rare Diseases 2010, 5:39 doi:10.1186/1750-1172-5-39