Related Research Articles
Applied ethics refers to the practical application of moral considerations. It is ethics with respect to real-world actions and their moral considerations in the areas of private and public life, the professions, health, technology, law, and leadership. For example, the bioethics community is concerned with identifying the correct approach to moral issues in the life sciences, such as euthanasia, the allocation of scarce health resources, or the use of human embryos in research. Environmental ethics is concerned with ecological issues such as the responsibility of government and corporations to clean up pollution. Business ethics includes questions regarding the duties or duty of 'whistleblowers' to the general public or their loyalty to their employers.
Casuistry is a process of reasoning that seeks to resolve moral problems by extracting or extending theoretical rules from a particular case, and reapplying those rules to new instances. This method occurs in applied ethics and jurisprudence. The term is also commonly used as a pejorative to criticize the use of clever but unsound reasoning, especially in relation to moral questions. It is the "[s]tudy of cases of conscience and a method of solving conflicts of obligations by applying general principles of ethics, religion, and moral theology to particular and concrete cases of human conduct. This frequently demands an extensive knowledge of natural law and equity, civil law, ecclesiastical precepts, and an exceptional skill in interpreting these various norms of conduct." It remains a common tool for applied ethics.

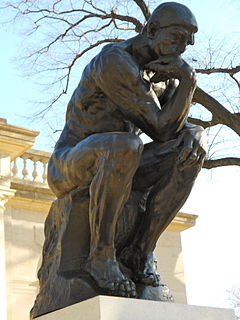
Ethics or moral philosophy is a branch of philosophy that "involves systematizing, defending, and recommending concepts of right and wrong behavior". The field of ethics, along with aesthetics, concerns matters of value; these fields comprise the branch of philosophy called axiology.
Bioethics is the study of the ethical issues emerging from advances in biology, medicine and technologies. It proposes the discussion about moral discernment in society and it is often related to medical policy and practice, but also to broader questions as environment and well-being. Bioethics is concerned with the ethical questions that arise in the relationships among life sciences, biotechnology, medicine, politics, law, theology and philosophy. It includes the study of values relating to primary care, other branches of medicine, ethical education in science, animal, and environmental ethics.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. It is important to note that these four values are not ranked in order of importance or relevance and that they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.

Virtue ethics are a class of normative ethical theories which treat the concept of moral virtue as central to ethics. Virtue ethics are usually contrasted with two other major approaches in normative ethics, consequentialism and deontology, which make the goodness of outcomes of an action (consequentialism) and the concept of moral duty (deontology) central. While virtue ethics does not necessarily deny the importance of goodness of states of affairs or moral duties to ethics, it emphasizes moral virtue, and sometimes other concepts, like eudaimonia, to an extent that other theories do not.
Utilitarian bioethics refers to the branch of bioethics that incorporates principles of utilitarianism to directing practices and resources where they will have the most usefulness and highest likelihood to produce happiness, in regards to medicine, health, and medical or biological research.
Applied philosophy is a branch of philosophy that studies philosophical problems of practical concern. The topic covers a broad spectrum of issues in environment, medicine, science, engineering, policy, law, politics, economics and education. The term was popularised in 1982 by the founding of the Society for Applied Philosophy by Brenda Almond, and its subsequent journal publication Journal of Applied Philosophy edited by Elizabeth Brake. Methods of Applied Philosophy are similar to other philosophical methods including questioning, dialectic, critical discussion, rational argument, systematic presentation, thought experiments and logical argumentation.
Joseph J. Fins, M.A.C.P., F.R.C.P. is an American physician and medical ethicist. He is chief of the Division of Medical Ethics at New York Presbyterian Hospital and Weill Cornell Medical College, where he serves as The E. William Davis Jr., M.D. Professor of Medical Ethics, and Professor of Medicine, Professor of Public Health, and Professor of Medicine in Psychiatry. Fins is also Director of Medical Ethics and an attending physician at New York Presbyterian Hospital-Weill Cornell Medical Center. Fins is also a member of the adjunct faculty of Rockefeller University and has served as Associate for Medicine at The Hastings Center. He was appointed by President Bill Clinton to The White House Commission on Complementary and Alternative Medicine Policy and currently serves on The New York State Task Force on Life and the Law by gubernatorial appointment.
The Declaration of Helsinki is a set of ethical principles regarding human experimentation developed originally in 1964 for the medical community by the World Medical Association (WMA). It is widely regarded as the cornerstone document on human research ethics.
The Johns Hopkins Berman Institute of Bioethics in Baltimore, Maryland, United States, is an interdisciplinary center serving the entire Johns Hopkins University and Health System. It is dedicated to the study of complex moral and policy issues in biomedical science, health care, and health policy. Established in 1995, the Institute seeks answers to ethical questions by promoting research in bioethics and encouraging moral reflection among a broad range of scholars, professionals, students, and citizens. Contributing to its mission are four divisions of the University: the Zanvyl Krieger School of Arts and Sciences, the Johns Hopkins School of Medicine, the Bloomberg School of Public Health, and the Johns Hopkins School of Nursing.
Donal O'Mathuna is Senior Lecturer in Ethics, Decision-Making & Evidence in the School of Nursing & Human Sciences at Dublin City University, Ireland, and Chair of the Academy of Fellows at the Center for Bioethics and Human Dignity in Chicago. His research interests include theology, alternative medicine and disaster ethics. He has written or edited several books, including Nanoethics: Big Ethical Issues with Small Technology (2009).
Albert R. Jonsen was one of the founders of the field of Bioethics. He was Emeritus Professor of Ethics in Medicine at the University of Washington, School of Medicine, where he was Chairman of the Department of Medical History and Ethics from 1987-1999. After retiring from UW, he returned to San Francisco where he co-founded the Program in Medicine and Human Values at Sutter Health's California Pacific Medical Center in 2003.
Mark Kuczewski is an American philosopher and bioethicist who has been a key contributor to the New Professionalism movement in medicine and medical education. In general, interest in professionalism has been widespread in medicine probably owing to the increasing regulatory and economic pressures on the practice of medicine. Many physicians have sought to identify the focal meaning of what it is to be a doctor in an effort to revitalize the profession. Kuczewski has been among a group that includes Richard and Sylvia Creuss, John Coulehan, and Matthew Wynia who see medical professionalism as including a commitment to social justice. That is, while professionalism entails such things as etiquette, communication skills, and basic medical ethics, professions are also expected to be leaders in educating the public and in advocating for the health of the public. Such leadership requires an understanding of the factors that lead some patient populations to be underserved and a commitment to bringing about social change to ameliorate these problems. The New Professionalism movement in medicine is a revival of communitarian bioethics that focus on the kinds of people and society we wish to be rather than on particular ethical questions of right and wrong. This focus on the relationship between the professional and the community can have important implications for medical education and professional development. While not eschewing case analysis and problem solving, the emphasis on the development of the person has created a renewed interest in narrative methods and reflection. Kuczewski has been an outspoken critic of efforts in medical education to focus on quantitative measures of professionalism education. He has argued that in an effort to make professionalism education “objective,” many medical educators are equating professionalism with trivial but easily measured behaviors. Kuczewski’s interest in professionalism and social justice has led him to pursue ethical issues in the interactions between medicine and recent immigrant populations. He has brought his work in communitarian and casuistic methods to bear on questions such as medical repatriation, insurance for undocumented immigrants, and the eligibility of DREAMers to become practicing physicians. His scholarship and advocacy was the catalyst for the Loyola University Chicago Stritch School of Medicine becoming the first medical school in the United States to explicitly welcome applications from DREAMers with Deferred Action for Childhood Arrivals (DACA) status. Under Kuczewski’s direction, the Neiswanger Institute for Bioethics and Health Policy at Loyola University Chicago has become a leader in educational programming to promote the relationship between medical professionalism and social justice. The Neiswanger Institute has contributed elements to the Stritch curriculum that explore the relationship between the business of medicine and social justice. The Institute also has online master of arts and doctoral programs that incorporating public health and leadership training in order to help health care professionals across the United States to promote service to the underserved. Kuczewski was elected president of the American Society for Bioethics and Humanities and served a two-year term from 2009 to 2011. The ASBH is the major professional association in the United States for individuals engaged in bioethics and medical humanities. During his term, the society aggressively began moving toward a process called Quality Attestation that will attest to the credentials and expected competence of clinical ethics consultants.
Ethics or moral philosophy is a branch of philosophy that involves systematizing, defending, and recommending concepts of right and wrong conduct. The field of ethics, along with aesthetics, concern matters of value, and thus comprise the branch of philosophy called axiology.
Jewish medical ethics is a modern scholarly and clinical approach to medical ethics that draws upon Jewish thought and teachings. Pioneered by Rabbi Immanuel Jakobovits in the 1950s, Jewish medical ethics centers mainly around an applied ethics drawing upon traditional rabbinic law (halakhah). In addition, scholars have begun examining theoretical and methodological questions, while the field itself has been broadened to encompass bioethics and non-halakhic approaches.

Principlism is an applied ethics approach to the examination of moral dilemmas that is based upon the application of certain ethical principles. This approach to ethical decision-making has been adopted enthusiastically in many different professional fields, largely because it sidesteps complex debates in moral philosophy at the theoretical level.
Clinical ethics support services initially developed in the United States of America, following court cases such as the Karen Ann Quinlan case, which stressed the need for mechanisms to resolve ethical disputes within health care. The Joint Commission on Accreditation of Healthcare Organizations requirement for hospitals, nursing homes, and home care agencies to have a standing mechanism to address ethical issues has also fostered this development.
Stephen Garrard Post has served on the Board of the John Templeton Foundation (2008-2014), which focuses on virtue and public life. He is a researcher, opinion leader, medical school professor, and best-selling author who has taught at the University of Chicago Medical School, Fordham University-Marymount, Case Western Reserve University School of Medicine (1988-2008) and Stony Brook University School of Medicine (2008-). He is widely known for his research on the ways in which giving can enhance the health and happiness of the giver, how empathy and compassionate care contribute to patient outcomes, ethical issues in caring for people with dementia, medical professionalism and the virtues, and positive psychology in relation to health and well-being. Post is an elected member of the College of Physicians of Philadelphia, the New York Academy of Medicine, and the Royal Society of Medicine, London. He was selected nationally as the Public Member of the United States Medical Licensing Examination (USMLE) Composite Committee (2000-2005), and was reappointed for outstanding contributions.
Primary care ethics is the study of the everyday decisions that primary care clinicians make, such as: how long to spend with a particular patient, how to reconcile their own values and those of their patients, when and where to refer or investigate, how to respect confidentiality when dealing with patients, relatives and third parties. All these decisions involve values as well as facts and are therefore ethical issues. These issues may also involve other workers in primary healthcare, such as receptionists and managers.
References
- ↑ Evidence based medicine and ethics. Hope T. J Med Ethics. 1995 October; 21(5): 259–260.
- ↑ Ethics and evidence based medicine. Kerridge I, Lowe M, Henry D. BMJ. 1998;316:1151-1153 (11 April).
- ↑ Argument-based medical ethics: A formal tool for critically appraising the normative medical ethics literature. McCullough LB, Coverdale JH, and Chervenak FA. AJOG. 191 (4): 1097-1102. October 2004.
- ↑ Evidence-Based Medical Ethics: Cases for Practice-Based Learning. Snyder, John E., Gauthier, Candace C. 2008, 240 p., Hardcover. ISBN 978-1-60327-245-2.
- ↑ Evidence-based ethics? On evidence-based practice and the "empirical turn" from normative bioethics. Goldenberg MJ. BMC Med Ethics. 2005 November;6(11): http://www.biomedcentral.com/1472-6939/6/11.