A medication is a drug used to diagnose, cure, treat, or prevent disease. Drug therapy (pharmacotherapy) is an important part of the medical field and relies on the science of pharmacology for continual advancement and on pharmacy for appropriate management.

A pharmacist, also known as a chemist in Commonwealth English, is a healthcare professional who specializes in the preparation, dispensing, and management of medications. A pharmacist provides pharmaceutical advice and guidance, often serving as a primary care provider in the community, and offering other services, such as health screenings and immunizations.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

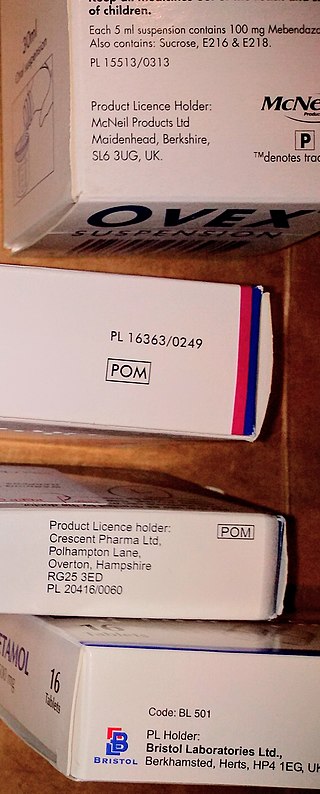
A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered healthcare professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin recipere, that gave the list of the materials to be compounded.
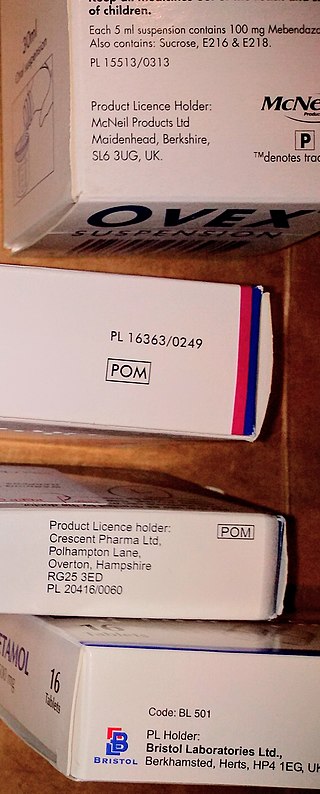
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.

The regulation of therapeutic goods, defined as drugs and therapeutic devices, varies by jurisdiction. In some countries, such as the United States, they are regulated at the national level by a single agency. In other jurisdictions they are regulated at the state level, or at both state and national levels by various bodies, as in Australia.
An essential medicines policy is one that aims at ensuring that people get good quality drugs at the lowest possible price, and that doctors prescribe the minimum of required drugs in order to treat the patient's illness. The pioneers in this field were Sri Lanka and Chile.
The Sri Lanka National Pharmaceuticals Policy was established in the 1970s following the submission of a report by Dr S.A. Wickremasinghe and Prof. Seneka Bibile. It aimed at ensuring that people get good quality drugs at the lowest possible price and that doctors would prescribe the minimum required drugs to treat the patient's illness. It was a pioneer in the field of rational National pharmaceuticals policy.
An online pharmacy, internet pharmacy, or mail-order pharmacy is a pharmacy that operates over the Internet and sends orders to customers through mail, shipping companies, or online pharmacy web portal.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.
Pharmacy in China involves the activities engaged in the preparation, standardization and dispensing of drugs, and its scope includes the cultivation of plants that are used as drugs, the synthesis of chemical compounds of medicinal value, and the analysis of medicinal agents. Pharmacists in China are responsible for the preparation of the dosage forms of drugs, such as tablets, capsules, and sterile solutions for injection. They compound physicians', dentists', and veterinarians' prescriptions for drugs. Pharmacological activities are also closely related to pharmacy in China.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Pharmaceutical fraud is when pharmaceutical companies engage in illegal, fraudulent activities to the detriment of patients and/or insurers. Examples include counterfeit drugs that do not contain the active ingredient, false claims in packaging and marketing, suppression of negative information regarding the efficacy or safety of the drug, and violating pricing regulations.
Online doctor is a term that emerged during the 2000s, used by both the media and academics, to describe a generation of physicians and health practitioners who deliver healthcare, including drug prescription, over the internet.
Antimicrobial stewardship (AMS) refers to coordinated efforts to promote the optimal use of antimicrobial agents, including drug choice, dosing, route, and duration of administration.
Pharmacy in the United Kingdom has been an integral part of the National Health Service since it was established in 1948. Unlike the rest of the NHS, pharmacies are largely privately provided apart from those in hospitals, and even these are now often privately run.
Separation of prescribing and dispensing, also called dispensing separation, is a practice in medicine and pharmacy in which the physician who provides a medical prescription is independent from the pharmacist who provides the prescription drug.

Drug utilization review refers to a review of prescribing, dispensing, administering and ingesting of medication. This authorized, structured and ongoing review is related to pharmacy benefit managers. Drug use/ utilization evaluation and medication utilization evaluations are the same as drug utilization review.