Related Research Articles

The sciatic nerve, also called the ischiadic nerve, is a large nerve in humans and other vertebrate animals. It is the largest branch of the sacral plexus and runs alongside the hip joint and down the lower limb. It is the longest and widest single nerve in the human body, going from the top of the leg to the foot on the posterior aspect. The sciatic nerve has no cutaneous branches for the thigh. This nerve provides the connection to the nervous system for the skin of the lateral leg and the whole foot, the muscles of the back of the thigh, and those of the leg and foot. It is derived from spinal nerves L4 to S3. It contains fibres from both the anterior and posterior divisions of the lumbosacral plexus.

The cauda equina is a bundle of spinal nerves and spinal nerve rootlets, consisting of the second through fifth lumbar nerve pairs, the first through fifth sacral nerve pairs, and the coccygeal nerve, all of which arise from the lumbar enlargement and the conus medullaris of the spinal cord. The cauda equina occupies the lumbar cistern, a subarachnoid space inferior to the conus medullaris. The nerves that compose the cauda equina innervate the pelvic organs and lower limbs to include motor innervation of the hips, knees, ankles, feet, internal anal sphincter and external anal sphincter. In addition, the cauda equina extends to sensory innervation of the perineum and, partially, parasympathetic innervation of the bladder.

Sciatica is pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Onset is often sudden following activities like heavy lifting, though gradual onset may also occur. The pain is often described as shooting. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes present. Weakness or numbness may occur in various parts of the affected leg and foot.

The quadriceps femoris muscle is a large muscle group that includes the four prevailing muscles on the front of the thigh. It is the sole extensor muscle of the knee, forming a large fleshy mass which covers the front and sides of the femur. The name derives from Latin four-headed muscle of the femur.
Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

Piriformis syndrome is a condition which is believed to result from nerve compression at the sciatic nerve by the piriformis muscle. It is a specific case of deep gluteal syndrome.

Cauda equina syndrome (CES) is a condition that occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged. Signs and symptoms include low back pain, pain that radiates down the leg, numbness around the anus, and loss of bowel or bladder control. Onset may be rapid or gradual.
Meralgia paresthetica or meralgia paraesthetica is pain or abnormal sensations in the outer thigh not caused by injury to the thigh, but by injury to a nerve which provides sensation to the lateral thigh.
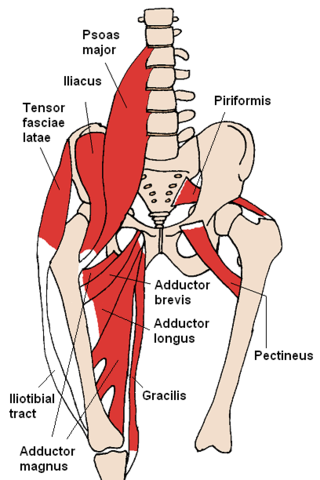
In the human body, the adductor longus is a skeletal muscle located in the thigh. One of the adductor muscles of the hip, its main function is to adduct the thigh and it is innervated by the obturator nerve. It forms the medial wall of the femoral triangle.
The rectus femoris muscle is one of the four quadriceps muscles of the human body. The others are the vastus medialis, the vastus intermedius, and the vastus lateralis. All four parts of the quadriceps muscle attach to the patella by the quadriceps tendon.

The iliopsoas muscle refers to the joined psoas major and the iliacus muscles. The two muscles are separate in the abdomen, but usually merge in the thigh. They are usually given the common name iliopsoas. The iliopsoas muscle joins to the femur at the lesser trochanter. It acts as the strongest flexor of the hip.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.

The femoral nerve is a nerve in the thigh that supplies skin on the upper thigh and inner leg, and the muscles that extend the knee. It is the largest branch of the lumbar plexus.
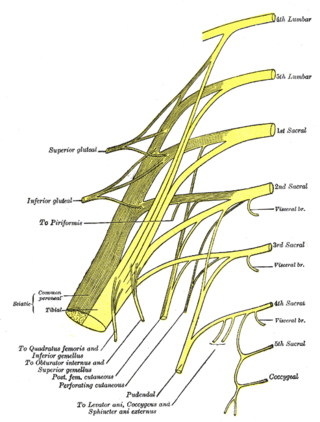
The inferior gluteal nerve is the main motor neuron that innervates the gluteus maximus muscle. It is responsible for the movement of the gluteus maximus in activities requiring the hip to extend the thigh, such as climbing stairs. Injury to this nerve is rare but often occurs as a complication of posterior approach to the hip during hip replacement. When damaged, one would develop gluteus maximus lurch, which is a gait abnormality which causes the individual to 'lurch' backwards to compensate lack in hip extension.

A spinal disc herniation is an injury to the intervertebral disc between two spinal vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatments may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

The straight leg raise is a test that can be performed during a physical examination, with the leg being lifted actively by the patient or passively by the clinician. If the straight leg raise is done actively by the patient, it is a test of functional leg strength, particularly the rectus femoris element of the quadriceps. If carried out passively, it is used to determine whether a patient with low back pain has an underlying nerve root sensitivity, often located at L5. The rest of this article relates to the passive version of the test.
Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from Latin claudicare 'to limp', refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.

The term sacroiliac joint dysfunction refers to abnormal motion in the sacroiliac joint, either too much motion or too little motion, that causes pain in this region.
Femoral nerve dysfunction, also known as femoral neuropathy, is a rare type of peripheral nervous system disorder that arises from damage to nerves, specifically the femoral nerve. Given the location of the femoral nerve, indications of dysfunction are centered around the lack of mobility and sensation in lower parts of the legs. The causes of such neuropathy can stem from both direct and indirect injuries, pressures and diseases. Physical examinations are usually first carried out, depending on the high severity of the injury. In the cases of patients with hemorrhage, imaging techniques are used before any physical examination. Another diagnostic method, electrodiagnostic studies, are recognized as the gold standard that is used to confirm the injury of the femoral nerve. After diagnosis, different treatment methods are provided to the patients depending upon their symptoms in order to effectively target the underlying causes. Currently, femoral neuropathy is highly underdiagnosed and its precedent medical history is not well documented worldwide.
References
- ↑ Ory, Avi (June 2007). "Dr Jacob Mackiewicz (1887-1966) and his sign". Journal of Medical Biography. 15 (2): 102–103. doi:10.1258/j.jmb.2007.06-16. PMID 17551611. S2CID 71610526 . Retrieved 14 February 2019.
- 1 2 3 Fritz, Julie (2012-01-01), Andrews, James R.; Harrelson, Gary L.; Wilk, Kevin E. (eds.), "17 - Low Back Rehabilitation", Physical Rehabilitation of the Injured Athlete (Fourth Edition), Philadelphia: W.B. Saunders, pp. 333–356, ISBN 978-1-4377-2411-0 , retrieved 2021-01-06
- ↑ Christodoulides, Antonios N (1989). "Ipsilateral Sciatica on Femoral Nerve Stretch Tests is Pathognomonic of and L4/5 Disc Protrusion". The Journal of Bone and Joint Surgery. 71 (1): 88–89. doi:10.1302/0301-620X.71B1.2915013. PMID 2915013. S2CID 6472889.