A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, tertiary care, and public health.

Community health refers to non-treatment based health services that are delivered outside hospitals and clinics. Community health is a subset of public health that is taught to and practiced by clinicians as part of their normal duties. Community health volunteers and community health workers work with primary care providers to facilitate entry into, exit from and utilization of the formal health system by community members as well as providing supplementary services such as support groups or wellness events that are not offered by medical institutions.
Allied health professions (AHPs) are a category of health professionals that provide a range of diagnostic, preventive, therapeutic, and rehabilitative services in connection with health care. While there is no international standard for defining the diversity of allied health professions, they are typically considered those which are distinct from the fields of medicine, nursing and dentistry.
A health professional, healthcare professional, or healthcare worker is a provider of health care treatment and advice based on formal training and experience. The field includes those who work as a nurse, physician, physician assistant, registered dietitian, veterinarian, veterinary technician, optometrist, pharmacist, pharmacy technician, medical assistant, physical therapist, occupational therapist, dentist, midwife, psychologist, audiologist, or healthcare scientist, or who perform services in allied health professions. Experts in public health and community health are also health professionals.

A nursing shortage occurs when the demand for nursing professionals, such as Registered Nurses (RNs), exceeds the supply locally—within a healthcare facility—nationally or globally. It can be measured, for instance, when the nurse-to-patient ratio, the nurse-to-population ratio, the number of job openings necessitates a higher number of nurses than currently available, or the current number of nurses is above a certain age where retirement becomes an option and plays a factor in staffing making the workforce in a higher need of nurses. The nursing shortage is global according to 2022 World Health Organization fact sheet.

Health policy can be defined as the "decisions, plans, and actions that are undertaken to achieve specific healthcare goals within a society". According to the World Health Organization, an explicit health policy can achieve several things: it defines a vision for the future; it outlines priorities and the expected roles of different groups; and it builds consensus and informs people.
Mid-level practitioners, also called non-physician practitioners, advanced practice providers, or commonly mid-levels, are health care providers who assess, diagnose, and treat patients but do not have formal education or certification as a physician. The scope of a mid-level practitioner varies greatly among countries and even among individual practitioners. Some mid-level practitioners work under the close supervision of a physician, while others function independently and have a scope of practice difficult to distinguish from a physician. The legal scope of practice for mid-level practitioners varies greatly among jurisdictions, with some having a restricted and well-defined scope, while others have a scope similar to that of a physician. Likewise, the training requirement for mid-level practitioners varies greatly between and within different certifications and licensures.

Global mental health is the international perspective on different aspects of mental health. It is 'the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide'. There is a growing body of criticism of the global mental health movement, and has been widely criticised as a neo-colonial or "missionary" project and as primarily a front for pharmaceutical companies seeking new clients for psychiatric drugs.

mHealth is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and personal digital assistants (PDAs), and wearable devices such as smart watches, for health services, information, and data collection. The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information. mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery/sharing of healthcare information for practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care as well as training and collaboration of health workers.

A community health worker (CHW) is a member of a community who provides basic health and medical care within their community, and is capable of providing preventive, promotional and rehabilitation care to that community, typically without formal education equal to that of a nurse, CHO, or doctor. They are chosen within the community to assist a train personnel community health extension worker who is train in college or schools of health. A community health extension worker (CHEW) is a specially trained professional who provides similar preventive, curative and rehabilitative health care and services to people where they live and work. CHEW are trained for three years and they graduate with a diploma, while the JCHEW are trained for two years and graduate with a certificate. Other terms for this type of health care provider include lay health worker, village health worker, community health aide, community health promoter, and health advisor.

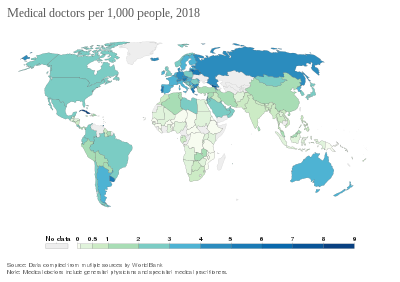
Physician supply refers to the number of trained physicians working in a health care system or active in the labor market. The supply depends primarily on the number of graduates of medical schools in a country or jurisdiction but also on the number continuing to practice medicine as a career path and remaining in their country of origin. The number of physicians needed in a given context depends on several different factors, including the demographics and epidemiology of the local population, the numbers and types of other health care practitioners working in the system, and the policies and goals in place of the health care system. If more physicians are trained than needed, supply exceeds demand. If too few physicians are trained and retained, some people may have difficulty accessing health care services. A physician shortage is a situation in which there are not enough physicians to treat all patients in need of medical care. That can be observed at the level of a given health care facility, a province/state, a country, or worldwide.
A human resource for health information system (HRHIS), also known as human resource information system (HRIS) — is a system for collecting, processing, managing and disseminating data and information on human resource for health (HRH). Depending on the level of development of a country's health care system and the organization of its workforce, an HRHIS can be computerized or paper-based, including information on numbers and distribution of health workers and track their career information. It is usually an integral part of a comprehensive health management information system, and may be used to monitor and assess the performance of the overall health system.

Unlicensed assistive personnel (UAP) are paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living (ADLs). UAPs also provide bedside care—including basic nursing procedures—all under the supervision of a registered nurse, licensed practical nurse or other health care professional. UAPs must demonstrate their ability and competence before gaining any expanded responsibilities in a clinical setting. While providing this care, UAPs offer compassion and patience and are part of the patient's healthcare support system. Communication between UAPs and registered nurses (RNs) is key as they are working together in their patients' best interests. The scope of care UAPs are responsible for is delegated by RNs or other clinical licensed professionals.
Human Resources for Health is a peer-reviewed open-access public health journal publishing original research and case studies on issues of information, planning, production, management, and governance of the health workforce, and their links with health care delivery and health outcomes, particularly as related to global health.
Healthcare in Malawi and its limited resources are inadequate to fully address factors plaguing the population, including infant mortality and the very high burden of diseases, especially HIV/AIDS, malaria and tuberculosis.
Society for Local Integrated Development Nepal is a nongovernmental, apolitical and nonprofit organization, established in 1997, that works to address certain complications like sexual and reproductive health problems, non-communicable diseases and other issues like crosscuts.
CapacityPlus is a global project funded by the United States Agency for International Development and led by IntraHealth International. Focused on strengthening the health workforce needed to achieve the Millennium Development Goals, the project assists countries to improve accessibility and quality of health services by addressing deficits in human resources for health (HRH).

The COVID-19 pandemic has impacted hospitals around the world. Many hospitals have scaled back or postponed non-emergency care. This has medical consequences for the people served by the hospitals, and it has financial consequences for the hospitals. Health and social systems across the globe are struggling to cope. The situation is especially challenging in humanitarian, fragile and low-income country contexts, where health and social systems are already weak. Health facilities in many places are closing or limiting services. Services to provide sexual and reproductive health care risk being sidelined, which will lead to higher maternal mortality and morbidity. The pandemic also resulted in the imposition of COVID-19 vaccine mandates in places such as California and New York for all public workers, including hospital staff.

The COVID-19 pandemic has impacted healthcare workers physically and psychologically. Healthcare workers are more vulnerable to COVID-19 infection than the general population due to frequent contact with positive COVID-19 patients. Healthcare workers have been required to work under stressful conditions without proper protective equipment, and make difficult decisions involving ethical implications. Health and social systems across the globe are struggling to cope. The situation is especially challenging in humanitarian, fragile and low-income country contexts, where health and social systems are already weak. Services to provide sexual and reproductive health care risk being sidelined, which will lead to higher maternal mortality and morbidity.