Related Research Articles
Algeria is the largest country in Africa and is estimated to have a population of around 40 million people. Algeria has a public health care system, which is accessible and free of charge to all citizens of Algeria. The public health care system is financed by the government of Algeria. Given Algeria's young population, policy favors preventive health care and clinics over hospitals. In keeping with this policy, the government maintains an intensive immunization programme and a policy which allows Algerian citizens health care for Hospitalisations, medicines and outpatient care free to all citizens of Algeria.

The Healthcare in Kazakhstan is a post-Soviet healthcare system under reform. The World Health Organization (WHO), in 2000, ranked the Kazakhstani healthcare system as the 64th in overall performance, and 135th by overall level of health.
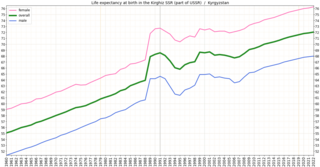
In the post-Soviet era, Kyrgyzstan's health system has suffered increasing shortages of health professionals and medicine. Kyrgyzstan must import nearly all its pharmaceuticals. The increasing role of private health services has supplemented the deteriorating state-supported system. In the early 2000s, public expenditures on health care decreased as a percentage of total expenditures, and the ratio of population to number of doctors increased substantially, from 296 per doctor in 1996 to 355 per doctor in 2001. A national primary-care health system, the Manas Program, was adopted in 1996 to restructure the Soviet system that Kyrgyzstan inherited. The number of people participating in this program has expanded gradually, and province-level family medicine training centers now retrain medical personnel. A mandatory medical insurance fund was established in 1997.

In terms of major health indicators, health in Paraguay ranks near the median among South American countries. In 2003 Paraguay had a child mortality rate of 29.5 deaths per 1,000 children, ranking it behind Argentina, Colombia, and Uruguay but ahead of Brazil and Bolivia. The health of Paraguayans living outside urban areas is generally worse than those residing in cities. Many preventable diseases, such as Chagas' disease, run rampant in rural regions. Parasitic and respiratory diseases, which could be controlled with proper medical treatment, drag down Paraguay's overall health. In general, malnutrition, lack of proper health care, and poor sanitation are the root of many health problems in Paraguay.
The Human Rights Measurement Initiative finds that Equatorial Guinea is fulfilling 43.5% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Equatorial Guinea achieves 64.4% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 58.8% of what is expected based on the nation's level of income. Equatorial Guinea falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 7.3% of what the nation is expected to achieve based on the resources (income) it has available.
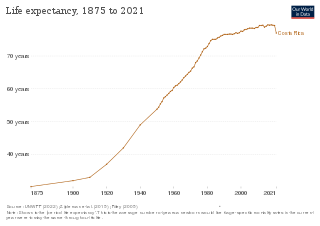
Costa Rica provides universal health care to its citizens and permanent residents. Both the private and public health care systems in Costa Rica are continually being upgraded. Statistics from the World Health Organization (WHO) frequently place Costa Rica in the top country rankings in the world for long life expectancy. WHO's 2000 survey ranked Costa Rica as having the 36th best health care system, placing it one spot above the United States at the time. In addition, the UN has ranked Costa Rica’s public health system within the top 20 worldwide and the number 1 in Latin America.

Life expectancy at birth in Belarus was 69 for men and 79 for women in 2016.
Public expenditure on health in the Gambia was at 1.8% of the GDP in 2004, whereas private expenditure was at 5.0%. There were 11 physicians per 100,000 persons in the early 2000s. Life expectancy at birth was 59.9 for females in 2005 and for males 57.7.
Mauritius had a life expectancy of 75.17 years in 2014. 39% of Mauritian men smoked in 2014. 13% of men and 23% of women were obese in 2008.
The Republic of the Congo faces a number of ongoing health challenges.
For the period between 2005 and 2010, El Salvador had the third-lowest birth rate in Central America, with 22.8 births per 1,000. However, during the same period, it had the highest death rate in Central America, 5.9 deaths per 1,000. In 2015 life expectancy for men were 67.8 years and 77.0 years for women. Healthy life expectancy was 57 for males and 62 for females in 2003. There was considerable improvement in socioeconomic and health status from 1990 to 2015. On June 22, 2020, the Hospital El Salvador, a permanent hospital conversion of the convention center in San Salvador, was opened to the public; it is Latin America's largest hospital and was built to receive COVID-19 patients.
Life expectancy in East Timor at birth was at 60.7 in 2007. The fertility rate is at six births per woman. Healthy life expectancy at birth was at 55 years in 2007.
The Human Rights Measurement Initiative finds that the Solomon Islands is fulfilling 78.8% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, the Solomon Islands achieves 100.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves 97.6% of what is expected based on the nation's level of income. Solomon Islands falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 38.9% of what the nation is expected to achieve based on the resources (income) it has available.
The Human Rights Measurement Initiative finds that Suriname is fulfilling 78.4% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Suriname achieves 94.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 83.2% of what is expected based on the nation's level of income. Suriname falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 57.9% of what the nation is expected to achieve based on the resources (income) it has available.

In 2016, life expectancy in Tunisia was 74 years for males and 78 years for females. By comparison, in the 1960s it was only 47.1 years. Infant mortality in 2017 was 12.1 per 1,000 live births.
Statistical overview of health status in Azerbaijan

Life expectancy in Albania was estimated at 77.59 years, in 2014, ranking 51st in the world, and outperforming a number of European Union countries, such as Hungary, Poland and the Czech Republic. In 2016 it was 74 for men and 79 for women. The most common causes of death are circulatory diseases followed by cancerous illnesses. Demographic and Health Surveys completed a survey in April 2009, detailing various health statistics in Albania, including male circumcision, abortion and more.
Life expectancy in Fiji is 66 years for men and 72 years for women. Maternal mortality was 59 per 100 000 live births in 2013.

The Human Rights Measurement Initiative finds that Maldives is fulfilling 72.0% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Maldives achieves 98.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves 99.7% of what is expected based on the nation's level of income. Maldives falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 18.2% of what the nation is expected to achieve based on the resources (income) it has available.
Expenditure on health in Samoa was 7.2% of GDP in 2014, US$418 per capita.
References
- ↑ "Human Rights Measurement Initiative – The first global initiative to track the human rights performance of countries". humanrightsmeasurement.org. Retrieved 2022-03-18.
- ↑ "Jamaica - HRMI Rights Tracker". rightstracker.org. Retrieved 2022-03-18.
- ↑ "Jamaica - HRMI Rights Tracker". rightstracker.org. Retrieved 2022-03-18.
- ↑ "Jamaica - HRMI Rights Tracker". rightstracker.org. Retrieved 2022-03-18.
- ↑ "Jamaica - HRMI Rights Tracker". rightstracker.org. Retrieved 2022-03-18.
- ↑ "Free Access To Health Care A Right For Every Jamaican – Holness". Gleaner. 10 October 2017. Retrieved 19 November 2018.
- ↑ "Free Health Care A Farce?". Gleaner. 7 December 2016. Retrieved 19 November 2018.
- ↑ "Health in Jamaica". Commonwealth Health. 2018. Retrieved 19 November 2018.
