Related Research Articles

The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication between the membranes, and also to create a pressure gradient.

Pulmonology, pneumology or pneumonology is a medical specialty that deals with diseases involving the respiratory tract. It is also known as respirology, respiratory medicine, or chest medicine in some countries and areas.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

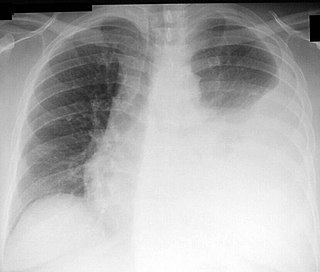
A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to Pneumothorax, or rarely in association with other conditions.

A chylothorax is an abnormal accumulation of chyle, a type of lipid-rich lymph, in the space surrounding the lung. The lymphatics of the digestive system normally returns lipids absorbed from the small bowel via the thoracic duct, which ascends behind the esophagus to drain into the left brachiocephalic vein. If normal thoracic duct drainage is disrupted, either due to obstruction or rupture, chyle can leak and accumulate within the negative-pressured pleural space. In people on a normal diet, this fluid collection can sometimes be identified by its turbid, milky white appearance, since chyle contains emulsified triglycerides.
Thoracentesis, also known as thoracocentesis, pleural tap, needle thoracostomy, or needle decompression, is an invasive medical procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia. The procedure was first performed by Morrill Wyman in 1850 and then described by Henry Ingersoll Bowditch in 1852.

Endoscopic ultrasound (EUS) or echo-endoscopy is a medical procedure in which endoscopy is combined with ultrasound to obtain images of the internal organs in the chest, abdomen and colon. It can be used to visualize the walls of these organs, or to look at adjacent structures. Combined with Doppler imaging, nearby blood vessels can also be evaluated.

A bronchopulmonary segment is a portion of lung supplied by a specific segmental bronchus and its vessels. These arteries branch from the pulmonary and bronchial arteries, and run together through the center of the segment. Veins and lymphatic vessels drain along the edges of the segment. The segments are separated from each other by layers of connective tissue that forms them into discrete anatomical and functional units. This separation means that a bronchopulmonary segment can be surgically removed without affecting the function of the others.
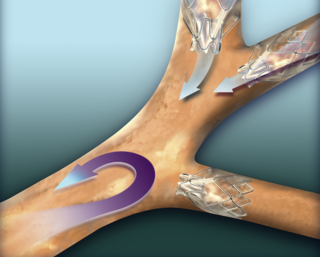
An endobronchial valve(EBV), is a small, one-way valve, which may be implanted in an airway feeding the lung or part of lung. The valve allows air to be breathed out of the section of lung supplied, and prevents air from being breathed in. This leaves the rest of the lung to expand more normally and avoid air-trapping. Endobronchial valves are typically implanted using a flexible delivery catheter advanced through a bronchoscope in minimally invasive bronchoscopic lung volume reduction procedures in the treatment of severe emphysema. The valves are also removable if they are not working properly.

Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment.
Lung cancer staging is the assessment of the extent to which a lung cancer has spread from its original source. As with most cancers, staging is an important determinant of treatment and prognosis. In general, more advanced stages of cancer are less amenable to treatment and have a worse prognosis.

A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less than three millimetres. There may also be multiple nodules.
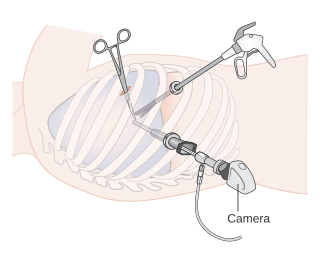
Video-assisted thoracoscopic surgery (VATS) is a type of minimally invasive thoracic surgery performed using a small video camera mounted to a fiberoptic thoracoscope, with or without angulated visualization, which allows the surgeon to see inside the chest by viewing the video images relayed onto a television screen, and perform procedures using elongated surgical instruments. The camera and instruments are inserted into the patient's chest cavity through small incisions in the chest wall, usually via specially designed guiding tubes known as "ports".
Electromagnetic navigation bronchoscopy (ENB) is a medical procedure utilizing electromagnetic technology designed to localize and guide endoscopic tools or catheters through the bronchial pathways of the lung. Using a virtual, three-dimensional (3D) bronchial map from a recently computed tomography (CT) chest scan and disposable catheter set, physicians are able to navigate to a desired location within the lung to biopsy lesions, stage lymph nodes, insert markers to guide radiotherapy or guide brachytherapy catheters.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

A lung biopsy is an interventional procedure performed to diagnose lung pathology by obtaining a small piece of lung which is examined under a microscope. Beyond microscopic examination for cellular morphology and architecture, special stains and cultures can be performed on the tissue obtained.
Thoracic endometriosis is a rare form of endometriosis where endometrial-like tissue is found in the lung parenchyma and/or the pleura. It can be classified as either pulmonary, or pleural, respectively. Endometriosis is characterized by the presence of tissue similar to the lining of the uterus forming abnormal growths elsewhere in the body. Usually these growths are found in the pelvis, between the rectum and the uterus, the ligaments of the pelvis, the bladder, the ovaries, and the sigmoid colon. The cause is not known. The most common symptom of thoracic endometriosis is chest pain occurring right before or during menstruation. Diagnosis is based on clinical history and examination, augmented with X-ray, CT scan, and magnetic resonance imaging of the chest. Treatment options include surgery and hormones.

Keertan Dheda MBBCh (Wits), FCP(SA), FCCP, PhD (Lond), FRCP (Lond), born in 1969, is a Professor of Mycobacteriology and Global health at the London School of Hygiene and Tropical Medicine (LSHTM) with an extra-mural joint appointment at the University of Cape Town (UCT), where he is a Professor of Respiratory Medicine.
Targeted lung denervation (TLD) is a procedure, that is currently being studied, to try to improve chronic obstructive pulmonary disease (COPD). Evidence to support its use is insufficient as of 2015. TLD is intended to block airway nerves of the parasympathetic nervous system to try to relax the airways. The procedure is done using a balloon catheter through a bronchoscope and uses radio frequency energy. The bronchoscope is passed through the person's mouth and into their lungs. A dual-cooled radiofrequency ablation catheter is passed through the bronchoscope to provide the treatment.
Bronchoscopic lung volume reduction(BLVR) is a procedure to reduce the volume of air within the lungs. BLVR was initially developed in the early 2000s as a minimally invasive treatment for severe COPD that is primarily caused by emphysema. BLVR evolved from earlier surgical approaches first developed in the 1950s to reduce lung volume by removing damaged portions of the lungs via pneumonectomy or wedge resection. Procedures include the use of valves, coils, or thermal vapour ablation.
References
- ↑ Ernst A.; Herth, F.J.F. Principles and Practice of Interventional Pulmonology. New York, NY: Springer 2013. ISBN 978-1-4614-4291-2.
- ↑ Jacobaeus HC. Ueber die Möglichkeit die Zystoskopie bei Untersuchungen seröser Höhlungen anzuwenden. Munch Med Wochenschr. 1910;57:2090–2019.
- ↑ Ernst A.; Herth, F.J.F. Principles and Practice of Interventional Pulmonology. New York, NY: Springer 2013. ISBN 978-1-4614-4291-2.
- ↑ Dumon, J; et al. Seven-Year Experience with the Dumon Prosthesis. Journal of Bronchology. 1996; 3:6-10.
- ↑ Pen Wang, K.; et al. Bronchoscopic needle aspiration biopsy of paratracheal tumors. American Review of Respiratory Disease. 1978. 117: 17-21.
- ↑ Silvestri, G. A.; et al. Methods for Staging Non-small Cell Lung Cancer: Diagnosis and Management of Lung Cancer, 3rd ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2013;143(5_suppl):e211S-e250S.
- ↑ "AABIP" . Retrieved 30 May 2017.
- ↑ "Journal of Bronchology & Interventional Pulmonology" . Retrieved 30 May 2017.
- ↑ "World Association for Bronchology and Interventional Pulmonology" . Retrieved 30 May 2017.
- 1 2 3 "AIPPD - Association of Interventional Pulmonology Program Directors" . Retrieved 30 May 2017.
- ↑ "Lahey Clinic Overview - Interventional Pulmonary Fellowship" . Retrieved 30 May 2017. With Harvard, Penn, & Duke also part of the early Founders of the field.
- ↑ Lee, H., L.; Mullon, J. J. Accredited Interventional Pulmonary Fellowships: The Time is Here. Journal of Bronchology & Interventional Pulmonology. 2015. 22: 189–190.
- ↑ Mullon, J.J.Interventional Pulmonology Fellowship Accreditation Standards: Executive Summary of the Multisociety Interventional Pulmonology Fellowship Accreditation Committee. Chest. 2017. 151:1114-1121.