Related Research Articles

Tetralogy of Fallot (TOF), formerly known as Steno-Fallot tetralogy, is a congenital heart defect characterized by four specific cardiac defects. Classically, the four defects are:

Dextrocardia is a rare congenital condition in which the apex of the heart is located on the right side of the body, rather than the more typical placement towards the left. There are two main types of dextrocardia: dextrocardia of embryonic arrest and dextrocardia situs inversus. Dextrocardia situs inversus is further divided.

Situs inversus is a congenital condition in which the major visceral organs are reversed or mirrored from their normal positions. The normal arrangement of internal organs is known as situs solitus. Although cardiac problems are more common, many people with situs inversus have no medical symptoms or complications resulting from the condition, and until the advent of modern medicine, it was usually undiagnosed.

dextro-Transposition of the great arteries is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.
The Fontan procedure or Fontan–Kreutzer procedure is a palliative surgical procedure used in children with univentricular hearts. It involves diverting the venous blood from the inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries. The procedure varies for differing congenital heart pathologies. For example in tricuspid atresia, the procedure can be done where the blood does not pass through the morphologic right ventricle; i.e., the systemic and pulmonary circulations are placed in series with the functional single ventricle. Whereas in hypoplastic left heart syndrome, the heart is more reliant on the more functional right ventricle to provide blood flow to the systemic circulation. The procedure was initially performed in 1968 by Francis Fontan and Eugene Baudet from Bordeaux, France, published in 1971, simultaneously described in July 1971 by Guillermo Kreutzer from Buenos Aires, Argentina, presented at the Argentinean National Cardilogy meeting of that year and finally published in 1973.
Situs ambiguus, or heterotaxy, is a rare congenital defect in which the major visceral organs are distributed abnormally within the chest and abdomen. Clinically heterotaxy spectrum generally refers to any defect of left-right asymmetry and arrangement of the visceral organs; however, classical heterotaxy requires multiple organs to be affected. This does not include the congenital defect situs inversus, which results when arrangement of all the organs in the abdomen and chest are mirrored, so the positions are opposite the normal placement. Situs inversus is the mirror image of situs solitus, which is normal asymmetric distribution of the abdominothoracic visceral organs. Situs ambiguus can also be subdivided into left-isomerism and right isomerism based on the defects observed in the spleen, lungs and atria of the heart.

Helen Brooke Taussig was an American cardiologist, working in Baltimore and Boston, who founded the field of pediatric cardiology. She is credited with developing the concept for a procedure that would extend the lives of children born with Tetralogy of Fallot. This concept was applied in practice as a procedure known as the Blalock-Thomas-Taussig shunt. The procedure was developed by Alfred Blalock and Vivien Thomas, who were Taussig's colleagues at the Johns Hopkins Hospital.
The Rastelli procedure is an open heart surgical procedure developed by Italian physician and cardiac surgery researcher, Giancarlo Rastelli, in 1967 at the Mayo Clinic, and involves using a pulmonary or aortic homograft conduit to relieve pulmonary obstruction in double outlet right ventricle with pulmonary stenosis.
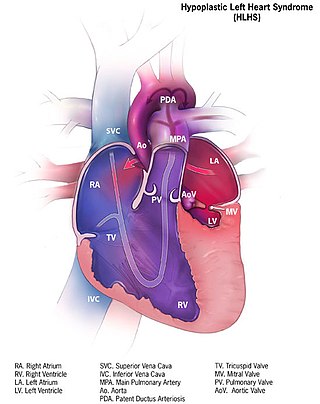
Hypoplastic left heart syndrome (HLHS) is a rare congenital heart defect in which the left side of the heart is severely underdeveloped and incapable of supporting the systemic circulation. It is estimated to account for 2-3% of all congenital heart disease. Early signs and symptoms include poor feeding, cyanosis, and diminished pulse in the extremities. The etiology is believed to be multifactorial resulting from a combination of genetic mutations and defects resulting in altered blood flow in the heart. Several structures can be affected including the left ventricle, aorta, aortic valve, or mitral valve all resulting in decreased systemic blood flow.

Pulmonary atresia is a congenital malformation of the pulmonary valve in which the valve orifice fails to develop. The valve is completely closed thereby obstructing the outflow of blood from the heart to the lungs. The pulmonary valve is located on the right side of the heart between the right ventricle and pulmonary artery. In a normal functioning heart, the opening to the pulmonary valve has three flaps that open and close.

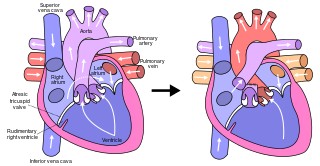
Tricuspid atresia is a form of congenital heart disease whereby there is a complete absence of the tricuspid valve. Therefore, there is an absence of right atrioventricular connection. This leads to a hypoplastic (undersized) or absent right ventricle. This defect is contracted during prenatal development, when the heart does not finish developing. It causes the systemic circulation to be filled with relatively deoxygenated blood. The causes of tricuspid atresia are unknown.

The Norwood procedure is the first of three surgeries intended to create a new functional systemic circuit in patients with hypoplastic left heart syndrome (HLHS) and other complex heart defects with single ventricle physiology. The first successful Norwood procedure involving the use of a cardiopulmonary bypass was reported by Dr. William Imon Norwood, Jr. and colleagues in 1981.
Taussig–Bing syndrome is a cyanotic congenital heart defect in which the patient has both double outlet right ventricle (DORV) and subpulmonic ventricular septal defect (VSD).

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA).

Atrial septostomy is a surgical procedure in which a small hole is created between the upper two chambers of the heart, the atria. This procedure is primarily used to palliate dextro-Transposition of the great arteries or d-TGA, a life-threatening cyanotic congenital heart defect seen in infants. It is performed prior to an arterial switch operation. Atrial septostomy has also seen limited use as a surgical treatment for pulmonary hypertension. The first atrial septostomy was developed by Vivien Thomas in a canine model and performed in humans by Alfred Blalock. The Rashkind balloon procedure, a common atrial septostomy technique, was developed in 1966 by American cardiologist William Rashkind at the Children's Hospital of Philadelphia.

The bidirectional Glenn (BDG) shunt, or bidirectional cavopulmonary anastomosis, is a surgical technique used in pediatric cardiac surgery procedure used to temporarily improve blood oxygenation for patients with a congenital cardiac defect resulting in a single functional ventricle. Creation of a bidirectional shunt reduces the amount of blood volume that the heart needs to pump at the time of surgical repair with the Fontan procedure.

Anomalous pulmonary venous connection is a congenital defect of the pulmonary veins.

Hypoplastic right heart syndrome (HRHS) is a congenital heart defect in which the structures on the right side of the heart, particularly the right ventricle, are underdeveloped. This defect causes inadequate blood flow to the lungs, and thus a cyanotic infant.
The Senning procedure is an atrial switch heart operation performed to treat transposition of the great arteries. It is named after its inventor, the Swedish cardiac surgeon Åke Senning (1915–2000), also known for implanting the first permanent cardiac pacemaker in 1958.

Pulmonary atresia with ventricular septal defect is a rare birth defect characterized by pulmonary valve atresia occurring alongside a defect on the right ventricular outflow tract.
References
- ↑ MITTAL, REKHA; PATHAK, KAMAL; MANOHARAN, S (April 1994). "ISOLATED LEVOCARDIA WITH SITUS INVERSUS (A Case Report)". Medical Journal Armed Forces India . 50 (2): 151–154. doi:10.1016/S0377-1237(17)31023-7. PMC 5529679 . PMID 28769192.
- ↑ Harris, Thomas R.; Rainey, Robert L. (1965-10-01). "Ideal isolated levocardia". American Heart Journal. 70 (4): 440–448. doi:10.1016/0002-8703(65)90354-6. PMID 5834189.
- ↑ Vijayakumar, V.; Brandt, T. (1991). "Prolonged survival with isolated levocardia and situs inversus". Cleveland Clinic Journal of Medicine. 58 (3): 243–247. doi:10.3949/ccjm.58.3.243. ISSN 0891-1150. PMID 1893555.
- ↑ "Isolated levocardia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2019-10-17.
- ↑ Vijayakumar, Vaniand, and Thomas Brandt (1991). "Prolonged survival with isolated levocardia and situs inversus". Cleveland Clinic Journal of Medicine. 58 (3): 243–247. doi:10.3949/ccjm.58.3.243. PMID 1893555.
- ↑ Hu, Jiaxin (2001). "The Diagnosis and Surgical Management of Levoversion and Isolated Levocardia". Academic Journal of Sun Yat-sen University of Medical Sciences.
- ↑ Gindes, L.; Hegesh, J.; Barkai, G.; Jacobson, J. M.; Achiron, R. (2007). "Isolated Levocardia: Prenatal Diagnosis, Clinical Importance, and Literature Review". Journal of Ultrasound in Medicine. 26 (3): 361–5. doi:10.7863/jum.2007.26.3.361. PMID 17324986.
- ↑ Gindes, Liat; Hegesh, Julian; Barkai, Gad; Jacobson, Jeffrey M.; Achiron, Reuven (2007). "Isolated Levocardia". Journal of Ultrasound in Medicine. 26 (3): 361–365. doi:10.7863/jum.2007.26.3.361. ISSN 1550-9613. PMID 17324986.
- ↑ Winer-Muram, Helen T. (1995). "Adult Presentation of Heterotaxic Syndromes and Related Complexes". Journal of Thoracic Imaging. 10 (1): 43–57. doi:10.1097/00005382-199501010-00004. ISSN 0883-5993. PMID 7891396. S2CID 25734073.
- ↑ "Hypoplastic Left Heart Syndrome Surgery: The Fontan Procedure (for Parents) - KidsHealth". kidshealth.org. Retrieved 2019-11-10.
- ↑ Young, Maurice D.; Griswold, Herbert E. (1951). "Situs Inversus of the Abdominal Viscera with Levocardia: Report of Eight Cases Submitted to the Blalock-Taussig Operation". Circulation. 3 (2): 202–214. doi: 10.1161/01.CIR.3.2.202 . ISSN 0009-7322. PMID 14812648.
- ↑ Young, Maurice D.; Griswold, Herbert E. (1951). "Situs Inversus of the Abdominal Viscera with Levocardia: Report of Eight Cases Submitted to the Blalock-Taussig Operation". Circulation. 3 (2): 202–214. doi: 10.1161/01.CIR.3.2.202 . ISSN 0009-7322. PMID 14812648.