Related Research Articles

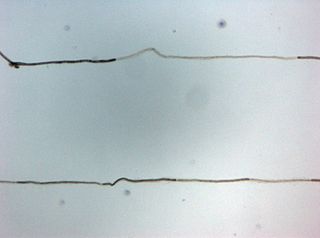
Myelin is a lipid-rich material that surrounds nerve cell axons to insulate them and increase the rate at which electrical impulses pass along the axon. The myelinated axon can be likened to an electrical wire with insulating material (myelin) around it. However, unlike the plastic covering on an electrical wire, myelin does not form a single long sheath over the entire length of the axon. Rather, myelin ensheaths the axon segmentally: in general, each axon is encased in multiple long sheaths with short gaps between, called nodes of Ranvier. At the nodes of Ranvier, which are approximately one thousandth of a mm (one micrometre in length, the axon's membrane is bare of myelin.

Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.

Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerve fibers are affected. Neuropathies affecting motor, sensory, or autonomic nerve fibers result in different symptoms. More than one type of fiber may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
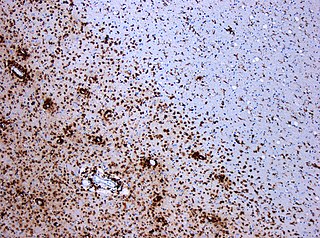
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Optic neuropathy is damage to the optic nerve from any cause. The optic nerve is a bundle of millions of fibers in the retina that sends visual signals to the brain.

Eva Lucille Feldman is an American physician-scientist known for her work in the field of neurodegenerative diseases. She serves as the James W. Albers Distinguished University Professor of Neurology[1] at the University of Michigan, as well as the Russell N. DeJong Professor of Neurology, Professor of Neurosurgery, and director of the NeuroNetwork for Emerging Therapies and ALS Center of Excellence at Michigan Medicine.
Guillain–Barré syndrome is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain often in the back along with muscle weakness, beginning in the feet and hands, often spreading to the arms and upper body. The symptoms may develop over hours to a few weeks. During the acute phase, the disorder can be life-threatening, with about 15% of people developing weakness of the breathing muscles requiring mechanical ventilation. Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure.
Progressive inflammatory neuropathy is a autoimmune disease that was identified in a report, released on January 31, 2008, by the Centers for Disease Control and Prevention. The first known outbreak of this neuropathy occurred in southeastern Minnesota in the United States. The disease was reported among slaughterhouse workers who appeared at various care facilities in the area reporting similar neurological symptoms. The disease was later identified at slaughterhouses in Indiana and Nebraska as well. The condition is characterized by acute paralysis, pain, fatigue, numbness, and weakness, especially in extremities. It was initially believed that workers might have contracted the disease through inhaling aerosols from pig brains that were created by a machine at the slaughterhouse and that an autoimmune response to the particles might have produced their mysterious peripheral neuropathy. These suspicions were confirmed in reports and investigations conducted at the Mayo Clinic in Rochester, Minnesota.
The Sir William Dunn School of Pathology is a department within the University of Oxford. Its research programme includes the cellular and molecular biology of pathogens, the immune response, cancer and cardiovascular disease. It teaches undergraduate and graduate courses in the medical sciences.

Kevin J. Tracey, a neurosurgeon and inventor, is the president and CEO of the Feinstein Institute for Medical Research, professor of neurosurgery and molecular medicine at the Zucker School of Medicine, and president of the Elmezzi Graduate School of Molecular Medicine in Manhasset, New York. The Public Library of Science Magazine, PLOS Biology, recognized Tracey in 2019 as one of the most cited researchers in the world.
Peter Kynaston "PK" Thomas was a Welsh academic neurologist, author, teacher and administrator. From 1974 to 1991 he was Professor of Neurology at the University of London. He was a fellow of University College London and the Royal Society of Medicine, and was the recipient of the Medal of the Association of British Neurologists. Thomas was, at various times, the president of the Association of British Neurologists, the European Neurological Society, and the Peripheral Nerve Society.
Clifford J. Woolf is professor of neurology and neurobiology at Harvard Medical School and director of the F.M. Kirby Neurobiology Center at Boston Children’s Hospital. He has added greatly to the understanding of pain.
Chronic relapsing inflammatory optic neuropathy (CRION) is a form of recurrent optic neuritis that is steroid responsive and dependent. Patients typically present with pain associated with visual loss. CRION is a clinical diagnosis of exclusion, and other demyelinating, autoimmune, and systemic causes should be ruled out. An accurate antibody test which became available commercially in 2017 has allowed most patients previously diagnosed with CRION to be re-identified as having MOG antibody disease, which is not a diagnosis of exclusion. Early recognition is crucial given risks for severe visual loss and because it is treatable with immunosuppressive treatment such as steroids or B-cell depleting therapy. Relapse that occurs after reducing or stopping steroids is a characteristic feature.

Stephen George Waxman is an American neurologist and neuroscientist. He served as Chairman of the Department of Neurology at Yale School of Medicine, and Neurologist-in-Chief at Yale-New Haven Hospital from 1986 until 2009. As of 2023, he is the Bridget Flaherty Professor of Neurology, Neurobiology, and Pharmacology at Yale University. He founded the Yale University Neuroscience & Regeneration Research Center in 1988 and is its director. He previously held faculty positions at Harvard Medical School, MIT, and Stanford Medical School. He is also visiting professor at University College London. He is the editor-in-chief of The Neuroscientist.
Eric Manvers Shooter was an English scientist known for investigating the biochemistry of nerve growth factor (NGF). From 1961 onwards he was affiliated with Stanford University School of Medicine, where he was founding chairman of the Department of Neurobiology (1975–1987).
David James Burke is an Australian neurologist and clinical neurophysiologist. He has held senior positions at the Prince of Wales Hospital, University of New South Wales and University of Sydney. He led one of two teams that formed the Prince of Wales Medical Research Institute, which was renamed Neuroscience Research Australia in 2010. His career has included a focus on the role of spinal cord circuits in the control of movement, the excitability of peripheral nerve axons in health and disease, and other areas of clinical neurophysiology.
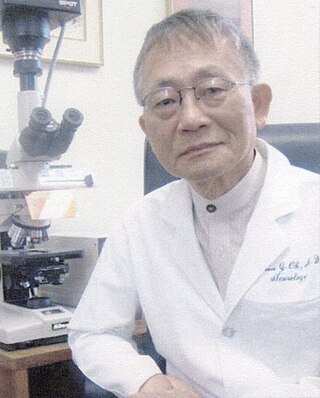
Shin Joong Oh is a South Korean and American physician who is Distinguished Professor of Neurology Emeritus at The University of Alabama at Birmingham in the United States. Oh is a clinician, researcher, and educator known for his contributions to the fields of neurology and electrodiagnostic medicine, particularly electromyography. He retired in 2014.
References
- ↑ The Flowering of a Waratah: A History of Australian Neurology and of the Australian Association of Neurologists (Hardcover)by Mervyn J. Eadie (Author)
- ↑ http://www.shsobu.org.au/wp-content/uploads/professors.pdf Archived 23 March 2019 at the Wayback Machine
- ↑ University of Sydney Biography
- ↑ A selection of refereed journal articles authored by Professor John D Pollard: